Immunity:这种基因突变导致1/4的人罹患癌症,并且还助力癌症生长!
2017-12-16 John,Juka 转化医学网
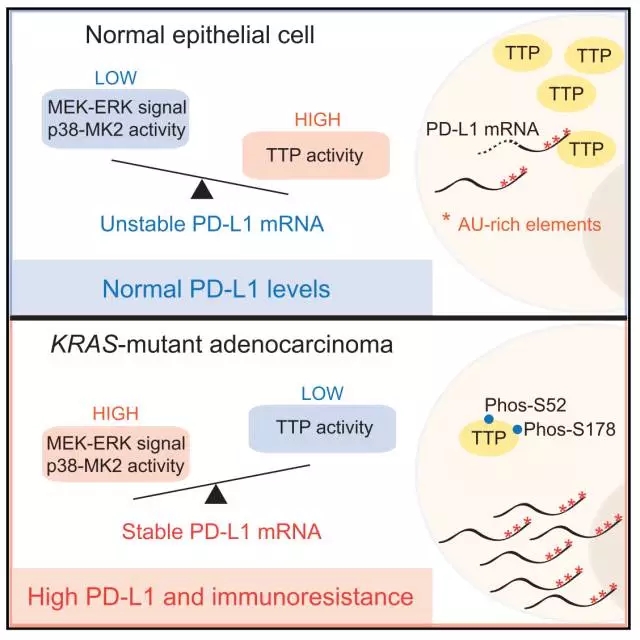
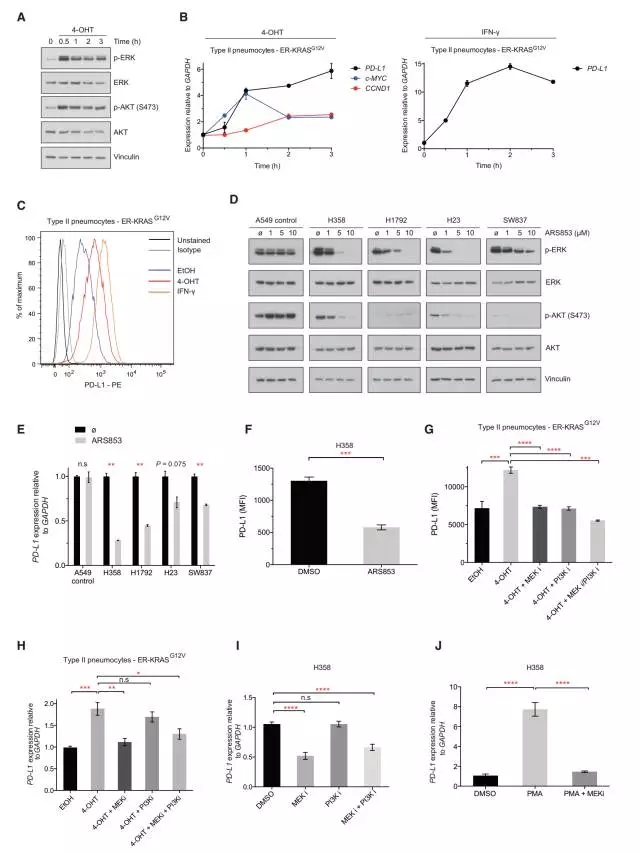
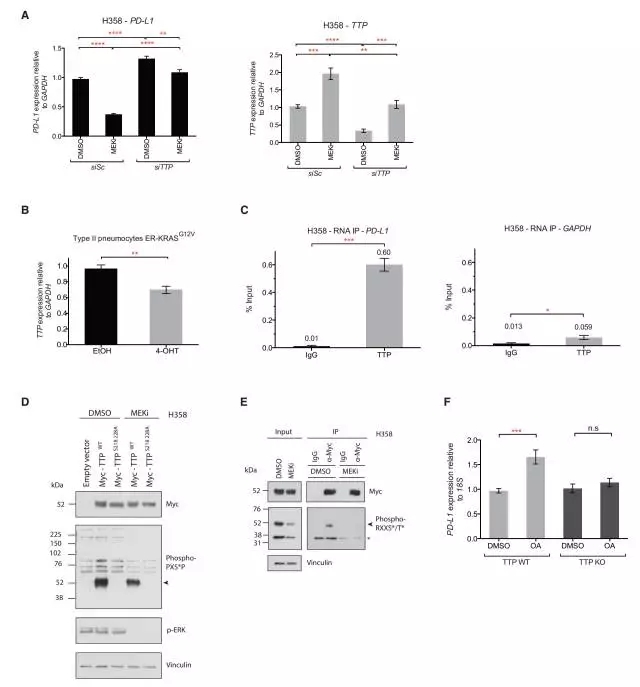
之前的相关研究表明,Ras基因是原癌基因,它发生突变以后就变成有致癌活性的癌基因。随着研究的继续深入,近日科学家发现,Ras基因的突变还可以抑制免疫系统的抗癌反应。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Immunity#
26
学习了
69
#患癌#
28
不错的文章值得推荐
68
好资料学习了!
66
学习一下
53