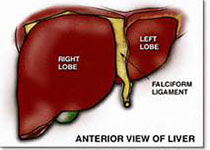
Hepatology:大连化物所所在肝癌诊断型代谢标志物研究中取得新进展
2017-10-10 尹沛源 大连化物所
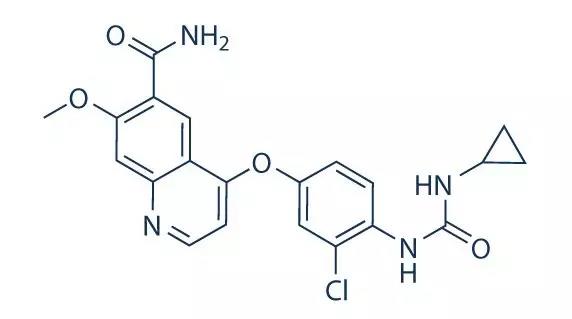
近日,中科院大连化学物理研究所高分辨分离分析及代谢组学研究组(1808组)在肝癌诊断型代谢标志物研究中取得新进展,相关结果发表在《Hepatology》杂志上。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#标志物#
24
#代谢标志物#
35
#EPA#
27
很好
28