葛均波等病例报告:回旋支远端闭塞但为何广泛ST段抬高?病因更致命!
2020-02-07 xujing 中国循环杂志
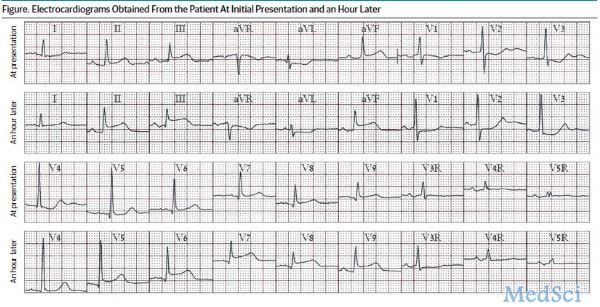
复旦大学附属中山医院葛均波院士团队在JAMA子刊介绍了一例突发性胸痛的老年女性患者的诊疗经验,从中,他们发现了导致广泛ST段抬高的一个比较少见的病因:亚急性左心室游离壁破裂。患者既往有糖尿病和阵发性房颤病史。入院心电图显示窦性心律正常,Ⅱ、Ⅲ和aVF导联ST段高达2.0 mm,V7-9导联ST段轻度下降,V2-4导联ST段下降1.0-2.0 mm。初始高敏感肌钙蛋白T水平为0.309 ng/ml。
入院心电图显示窦性心律正常,Ⅱ、Ⅲ和aVF导联ST段高达2.0 mm,V7-9导联ST段轻度下降,
V2-4导联ST段下降1.0-2.0 mm。
初始高敏感肌钙蛋白T水平为0.309 ng/ml。
患者的心率和血压正常。
不愿意接受急诊冠状动脉造影。
1小时后,患者疼痛加剧,更多导联出现ST段抬高,无病理性Q波。
心电图提示的受累区域和伴随的心源性休克不能用左回旋支远端的血栓性闭塞来解释,这意味着除了STEMI之外还有另一个原因。
为提升血压,使用了血管活性药物。
由于闭塞病变血管直径很小,通过导丝通道恢复血流,未进行球囊成形术和支架置入术。
然而,胸痛并没有消失。
为排除急性主动脉夹层,进行了血管造影,意外发现心肌和心包积液中存在造影剂。
诊断为亚急性左心室游离壁破裂。
很遗憾,病人死亡。
笔者指出,在STEMI早期,ST段抬高合并胸痛的鉴别诊断包括复发性血栓闭塞、冠状动脉痉挛和心包并发症。
亚急性左心室游离壁破裂合并AMI是梗死相关导联ST段抬高的少见原因。
发生AMI时,如果出现新的ST段抬高,且反复胸痛和新发低血压,应警惕亚急性左心室游离壁破裂。
如果怀疑左心室游离壁破裂,应紧急进行床边经胸超声心动图检查心包积液。
来源:
Hongyi?Wu,?Juying?Qian,?Junbo?Ge. An Unusual Cause of New Electrocardiographic ST-Segment Elevation. JAMA Intern Med. Published online February 3, 2020.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#回旋支远端闭塞#
18
#病例报告#
26
#ST段抬高#
22
#ST段#
40