原发性血小板增多症诊断与治疗中国专家共识(2016年版)
2016-11-03 佚名 中华血液学杂志
为了进一步规范我国血液科医师对原发性血小板增多症(ET)患者的临床诊治,由中华医学会血液学分会白血病淋巴瘤学组牵头,在广泛征求国内专家意见的基础上,最终达成了ET的诊断程序、实验室检查、诊断标准和治疗原则等方面的共识。一、诊断程序1.病史采集:必须仔细询问患者年龄,有无血管性头痛、头晕、视物模糊、肢端感觉异常和手足发绀等微循环障碍症状,有无疲劳、腹部不适、皮肤瘙痒、盗汗、骨痛、体重下降等情况,
为了进一步规范我国血液科医师对原发性血小板增多症(ET)患者的临床诊治,由中华医学会血液学分会白血病淋巴瘤学组牵头,在广泛征求国内专家意见的基础上,最终达成了ET的诊断程序、实验室检查、诊断标准和治疗原则等方面的共识。
一、诊断程序
1.病史采集:
必须仔细询问患者年龄,有无血管性头痛、头晕、视物模糊、肢端感觉异常和手足发绀等微循环障碍症状,有无疲劳、腹部不适、皮肤瘙痒、盗汗、骨痛、体重下降等情况,有无心血管高危因素(如高血压、高血脂、糖尿病、吸烟和充血性心力衰竭),有无血管栓塞病史(中风、短暂性缺血发作、心肌梗死、外周动脉血栓和下肢静脉、肝静脉、门静脉和肠系膜静脉等深静脉血栓),家族有无类似患者等。建议在初诊时及治疗过程中评估患者疗效时采用骨髓增殖性肿瘤总症状评估量表(MPN-SAF TSS)对患者进行症状负荷评估。
2.实验室检查:
以下实验室检查应作为疑诊ET患者的必检项目:①外周血细胞计数;②骨髓穿刺涂片和外周血涂片分类计数;③骨髓活检病理细胞学分析和网状纤维(嗜银)染色;④JAK2、CALR和MPL基因突变检测;⑤BCR-ABL融合基因;⑥C反应蛋白(CRP)、红细胞沉降率、血清铁、转铁蛋白饱和度、总铁结合力和血清铁蛋白;⑦肝脏、脾脏超声或CT检查。
二、诊断标准
1.ET诊断标准:
建议采用WHO(2016)诊断标准:符合4条主要标准或前3条主要标准和次要标准即可诊断ET。主要标准:①血小板计数(PLT)≥ 450×109/L;②骨髓活检示巨核细胞高度增生,胞体大、核过分叶的成熟巨核细胞数量增多,粒系、红系无显著增生或左移,且网状纤维极少轻度(1级)增多;③不能满足BCR-ABL+慢性髓性白血病、真性红细胞增多症(PV)、原发性骨髓纤维化(PMF)、骨髓增生异常综合征和其他髓系肿瘤的WHO诊断标准;④有JAK2、CALR或MPL基因突变。次要标准:有克隆性标志或无反应性血小板增多的证据。
2.ET后骨髓纤维化(post-ET MF)诊断标准:
采用骨髓纤维化研究和治疗国际工作组(IWG-MRT)标准[8]:主要标准(2条均需符合):①此前按WHO诊断标准确诊为ET;②骨髓活检示纤维组织分级为2/3级(按0~3级标准)或3/4级(按0~4级标准)。次要标准(至少需符合2条):①贫血或血红蛋白含量较基线水平下降20 g/L;②外周血出现幼粒幼红细胞;③进行性脾脏肿大(超过左肋缘下5 cm或新出现可触及的脾脏肿大);④以下3项体质性症状中至少出现1项:过去6个月内体重下降>10%,盗汗,不能解释的发热(>37.5 ℃)。
三、鉴别诊断
1.反应性血小板增多症:
最常见的反应性血小板增多的原因有感染、炎症和缺铁性贫血等。感染和炎症常有CRP和红细胞沉降率增高,因此,一个血小板增多的患者应通过这2项检查结合病史首先应排除感染和炎症导致的反应性血小板增多。缺铁性贫血时可有血小板增多,可通过血清铁等检查鉴别。如果患者有缺铁,在充分铁剂补充治疗后再复查血常规。
2.其他伴血小板增多的血液系统疾病:
PV、PMF、慢性髓性白血病、慢性粒单核细胞白血病、骨髓增生异常综合征中的5q-综合征、骨髓增生异常综合征/骨髓增殖性肿瘤伴环状铁粒幼红细胞和血小板增多(MDS/MPN-RS-T)等血液系统疾病均可出现血小板增多,ET应与这些疾病进行鉴别诊断。骨髓病理对于鉴别ET与隐匿性PV(masked-PV)和纤维化前期(prefibritic)骨髓纤维化至关重要,这依赖于经严格专业培训且经验丰富的血液病理科医师。ET骨髓增生程度正常,以巨核细胞增生为主,粒系和红系增生正常且无左移,巨核细胞呈随机分布或呈松散簇,巨核细胞体积大或巨大,胞核过分叶(鹿角状),胞质成熟正常。masked-PV骨髓增生程度经年龄调整后为轻至中度增生,主要是巨核细胞和红系细胞增生,巨核细胞大小不一,成熟正常。纤维化前期骨髓纤维化患者骨髓呈极度增生,以粒细胞和巨核细胞增生为主,红系细胞增生常为轻至中度减低,巨核细胞大小不一,成簇分布,胞核低分叶,染色质凝集(呈气球状或云朵状),核/胞质比增大(成熟障碍),裸核巨核细胞数增多。
四、预后判断标准
1.ET血栓国际预后积分(IPSET-thrombosis)系统:
血栓是影响ET患者生活质量和降低患者寿命的主要原因。患者确诊ET后首先应按IPSET-thrombosis系统对患者发生血栓的风险作出评估:年龄>60岁(1分),有心血管危险因素(CVR)(1分),此前有血栓病史(2分),Jak2V617F突变阳性(2分)。依累计积分血栓危度分组:低危(0~1分)、中危(2分)和高危(≥3分)。各危度组患者血栓的年发生率分别为1.03%、2.35%和3.56%。
2.ET国际预后积分(IPSET)系统:
建议采用IWG-MRT提出的IPSET对患者总体生存预后作出评估:年龄(<60岁0分;≥60岁,2分);白细胞计数(<11×109/L 0分,≥11×109/L,1分);血栓病史(无0分,有1分)。依累计积分预后危度分组:低危组(0分),中危组(1~2分),高危组(≥3分)。各危度组患者中位生存期依次为没有达到、24.5年和13.8年。
五、治疗
ET的治疗目标是预防和治疗血栓合并症,因此,现今治疗的选择主要是依据患者血栓风险分组来加以制定。血小板计数应控制在<600 × 109/L,理想目标值为400×109/L。
1.治疗选择的原则:
(1)无血栓病史:①年龄<60岁、无CVR或JAK2V617突变者,可采用观察随诊策略;②年龄< 60岁、有CVR或JAK2V617突变者,给予阿司匹林100 mg每日1次;③年龄<60岁、有CVR和JAK2V617突变且PLT<1000×109/L者,给予阿司匹林100 mg每日1次;④年龄≥60岁、无CVR或JAK2V617突变者给予降细胞治疗+阿司匹林100 mg每日1次;⑤年龄≥60岁、有CVR或JAK2V617突变者给予降细胞治疗+阿司匹林100 mg每日2次;⑥任何年龄、PLT>1 500×109/L的患者,给予降细胞治疗。
(2)有动脉血栓病史:①任何年龄、无CVR和JAK2V617突变者,给予降细胞治疗+阿司匹林100 mg每日1次;②年龄≥60岁、有CVR或JAK2V617突变者,给予降细胞治疗+阿司匹林100 mg每日2次。
(3)有静脉血栓病史:①任何年龄、无CVR和JAK2V617突变者,给予降细胞治疗+系统抗凝治疗;②任何年龄、有CVR或JAK2V617突变的患者,给予降细胞治疗+系统抗凝治疗+阿司匹林100 mg每日1次。
(4)治疗选择的动态调整:在病程中应对患者进行动态评估并根据评估结果调整治疗选择。PLT >1000×109/L的患者服用阿司匹林可增加出血风险,应慎用。PLT >1500×109/L的患者不推荐服用阿司匹林。对阿司匹林不耐受的患者可换用氯吡格雷。
(5)有CVR的患者,应积极进行相关处理(戒烟,高血压患者控制血压,糖尿病患者控制血糖等)。
2.降细胞治疗一线药物:
(1)羟基脲:起始剂量为15~20 mg·kg-1·d-1,8周内80%患者的血小板计数可降至500×109/L以下,然后给予适当的维持剂量治疗。血常规监测:治疗的前2个月每周1次,以后每月1次,血象稳定后每3个月1次。对羟基脲耐药或不耐受的患者可换用干扰素或阿拉格雷等二线药物。
(2)干扰素:为年龄<40岁患者的首选治疗药物。起始剂量为300万U/d皮下注射,起效后调整剂量,最低维持剂量为300万U每周1次。醇化干扰素的起始剂量为0.5 μg/kg每周1次,12周后如无疗效可增量至1.0 μg/kg每周1次。部分患者在使用干扰素后可出现甲状腺功能减低、抑郁等精神症状,因此在使用干扰素前应进行甲状腺功能检查,仔细询问患者是否有精神病史。血常规监测:治疗的第1个月每周1次,第2个月每2周1次,以后每月1次,血象稳定后每3个月1次。
3.降细胞治疗二线药物:
(1)阿拉格雷:起始剂量为0.5 mg每日2次口服,至少1周后开始调整剂量,维持PLT<600× 109/L。剂量增加每周不超过0.5 mg/d,最大单次剂量为2.5 mg,每日最大剂量为10 mg,PLT维持在(150~400)×109/L为最佳。
(2)白消安、双溴丙哌嗪和32P:由于这些药物的最严重不良反应是远期发生治疗相关性白血病或骨髓增生异常综合征及肿瘤,现仅作为老年患者的二线药物选择。
4.妊娠期ET患者的治疗:
约20%的ET患者确诊时年龄<40岁。ET患者妊娠会出现流产、早产、胎儿发育迟缓等。此外,妊娠会增加ET患者出血和血栓的风险,因此,应给予特殊处理。
服用羟基脲治疗的患者(无论男、女)在受孕前至少应有3个月的洗脱期。女性患者受孕前应仔细评估是否有以下妊娠合并症高危因素:①此前有动、静脉血栓病史(无论是否妊娠);②此前有ET导致的出血病史(无论是否妊娠);③此前发生过以下可能由ET引起的妊娠合并症:反复发生的非孕妇和胎盘因素所致妊娠10周内流产,不能解释的宫内胎儿发育迟缓,妊娠≥10周胎儿发育正常的宫内死胎,因严重先兆子痫或胎盘功能不全导致妊娠<34周且胎儿发育正常的早产、胎盘剥离、严重的产前和产后出血(需要红细胞输注)等;④血小板计数显著增高(PLT>1500×109/L)。ET孕妇的孕期监护应由血液科医师与产科医师共同完成。
无妊娠合并症高危因素的孕妇,给予阿司匹林100 mg每日1次;有妊娠合并症高危因素的孕妇,给予阿司匹林每日1次(出血则停用)联合低分子肝素(4000 U/d)至产后6周,PLT≥1 500×109/L时加用干扰素(建议首选醇化干扰素)。
5.post-ET MF和白血病转变患者的治疗:
post-ET MF的治疗参照《原发性骨髓纤维化诊断与治疗中国专家共识(2015年版)》。白血病转变患者按相应指南进行处理。
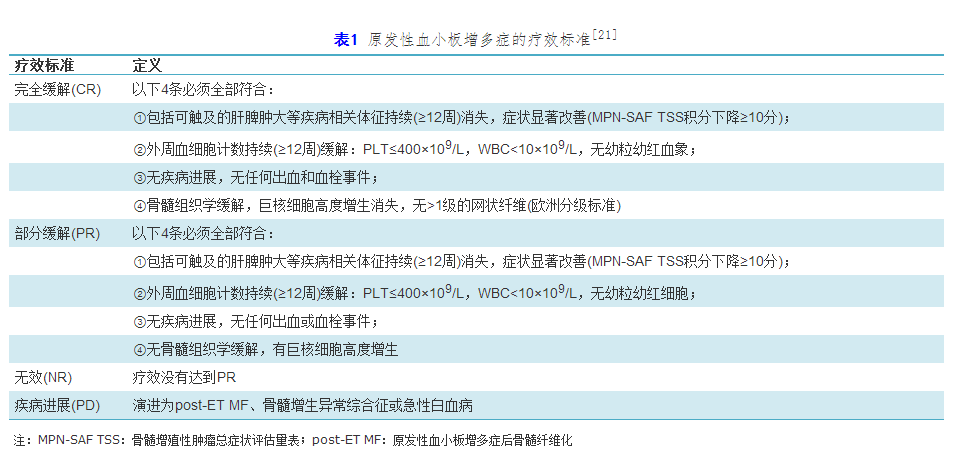
六、疗效判断标准
采用欧洲白血病网和IWG-MRT 2013年修订的ET疗效评价标准(表1),主要包括临床血液学及骨髓组织学评价两方面。分子生物学疗效对于评价完全缓解(CR)或部分缓解(PR)不是必需的。完全分子生物学缓解(CRm):原先存在的异常完全消失。部分分子生物学缓解:基线等位基因突变负荷≥20%的患者治疗后等位基因突变负荷下降≥50%。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









没有出处的文献.不完整.
59
#专家共识#
33
#诊断与治疗#
29
#中国专家共识#
32
#原发性#
31
收藏
53
#血小板增多症#
34
#原发性血小板增多症#
40