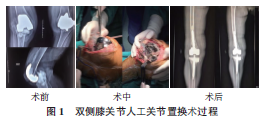
双侧膝关节人工关节置换术后相继感染1例
2019-10-11 张晨 宋国瑞 刘子歌 宁夏医科大学学报
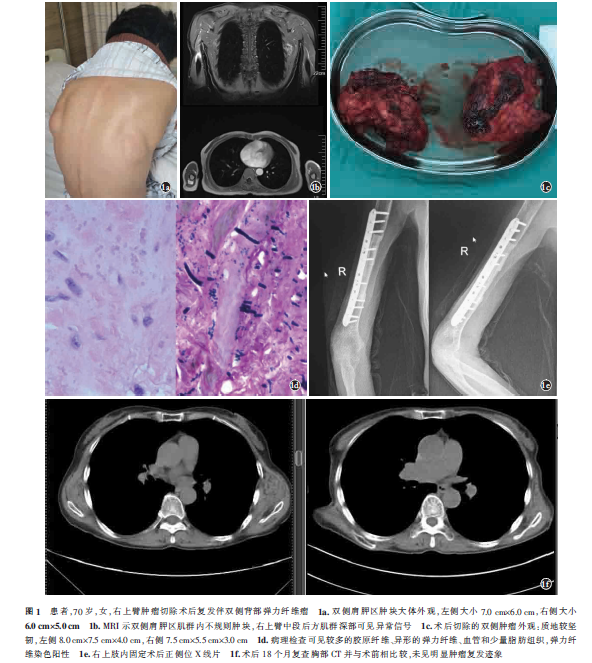
患者,女性,62 岁,因“左膝关节置换术后疼痛半年,加重伴流脓1 月,右膝关节旷置术后疼痛伴活动受限2 月”入住宁夏医科大学总医院脊柱骨科。患者15 年前无诱因下出现双膝关节疼痛不适,2008 年患者自觉上述症状加重并出现双膝关节活动受限,至宁夏武警医院就诊,于2008 年6 月8 日行“左膝关节置换术”,2013 年12 月13 日于宁夏武警医院行“右侧人工膝关节置换术”。2016 年患者无明显
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#置换#
26
#人工关节#
33
#关节置换术#
35
#双侧#
36
#置换术#
46