Diabetes Care.:减重手术对早发性肥胖有效
2020-03-13 国际糖尿病 idiabetes
越来越多的证据表明减重手术可以持续减轻体重、改善伴随疾病和延长生存期。早发性肥胖症患者和成年肥胖症患者接受减重手术是否同样获益呢?根据Diabetes Care发表的一项研究结果表明,20岁之前患肥胖
越来越多的证据表明减重手术可以持续减轻体重、改善伴随疾病和延长生存期。早发性肥胖症患者和成年肥胖症患者接受减重手术是否同样获益呢?根据Diabetes Care发表的一项研究结果表明,20岁之前患肥胖症且接受减重手术的成年人可能会获益更多。
研究概要
瑞典哥德堡大学Johanna C. Andersson-Assarsson博士团队评估了37岁至60岁之间接受减重手术的2007例患者及与其对照的未接受减重手术的2040例患者的体重变化及2型糖尿病、微血管和心血管疾病进展。受试者自述了20岁时的体重,研究人员根据这些数据将接受减重手术的患者分为早期肥胖组(BMI 30 kg/㎡;n=528;平均年龄44.9岁;女性68.6%),早期超重组(BMI 25-29.99 kg/㎡; n =744;平均年龄47岁; 女性69.5%)和早期正常体重组(BMI<25kg/㎡,n=725,平均年龄49岁,女性73.8%)。未接受减重手术者进行相同分组:早期肥胖组(n=439,平均年龄46.1岁,女性70.2%),早期超重组(n=721,平均年龄48.7岁,女性68.9%)和早期正常体重组(n = 869,平均年龄 50岁,女性73.2%)。
研究人员在术后6个月随访受试者,之后4年每年随访一次,之后6年每两年随访一次。每次随访时评估体重,同时使用瑞典死因登记和国家患者登记确诊2型糖尿病、微血管和心血管并发症。
主要结果
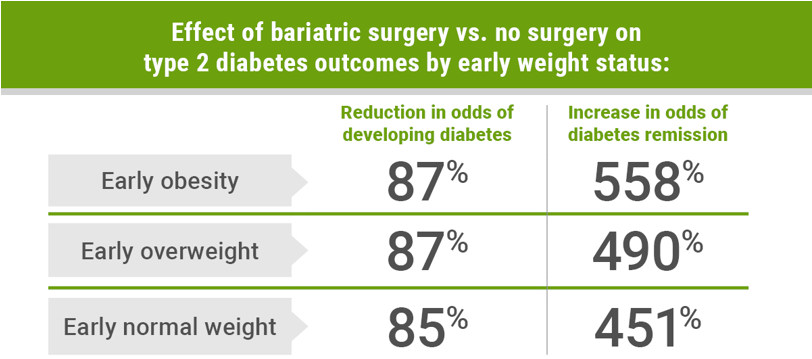
接受手术治疗的早期肥胖症患者与未接受手术者相比,术后10年内发生2型糖尿病的危险降低了87%(OR = 0.13; 95%CI:0.07~0.025),而早期超重者(OR=0.13 ;95%CI,0.08-0.22)和早期正常体重者(OR =0.15;95%CI:0.09-0.24)罹患此病的风险也都降低。
相反,接受手术治疗且患有2型糖尿病的早期肥胖症患者与未接受手术者相比,术后10年内更容易进入糖尿病缓解期(OR=5.58;95%CI:1.11-27.96),早期超重者(OR=4.9; 95%CI:1.69-14.17)和早期正常体重者(OR=4.51; 95%CI:1.58-12.86)也是如此。
对于接受手术的早期肥胖患者,无论是否存在2型糖尿病(HR=0.4;95%CI:0.22-0.73)与未接受手术的患者相比,微血管并发症的风险也显著降低(HR=0.39;95%CI:0.23-0.66)。
Andersson-Assarsson评述到:“我们本来预期早发性肥胖组接受减重手术后体重减轻少、预防肥胖症合并症效果差,但并非如此。早发性肥胖组较成年肥胖者体重减轻甚至稍微多,糖尿病缓解,微血管并发症或糖尿病、心血管疾病和癌症的发生率没有差异。”
原始出处:
Kristensson FM, et al. Effects of Bariatric Surgery in Early- and Adult-Onset Obesity in the Prospective Controlled Swedish Obese Subjects Study. Diabetes Care. 2020;doi:10.2337/dc19-1909.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
40
#早发#
43
#DIA#
32
#Diabetes#
40
学习了
88