锁骨远端解剖钢板倒置治疗胸锁关节前脱位1例
2019-09-08 申东 谢文鹏 毕荣修 世界最新医学信息文摘
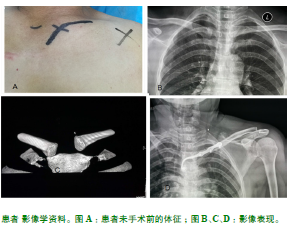
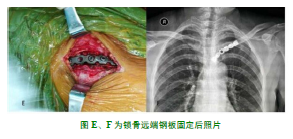
我们2018收治胸锁关节前脱位病人一例。具体病情如下:患者女,43岁,因外伤致左侧胸前区疼痛,查体见胸骨柄左侧有骨性突起,局部压痛(+),各个方向的左上肢主动运动均可引起疼痛加剧,在完善相关影响检查后,于我院行胸锁钩钢板内固定治疗,后自述因过早剧烈体力劳动致使患处再次疼痛且可见固定突起,遂进行第二次手术,将内固定物取出并行锁骨远端解剖钢板倒置内固定。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#钢板倒置#
43
#前脱位#
46
#远端解剖#
40
#锁骨远端#
61
#锁骨#
0
#脱位#
37