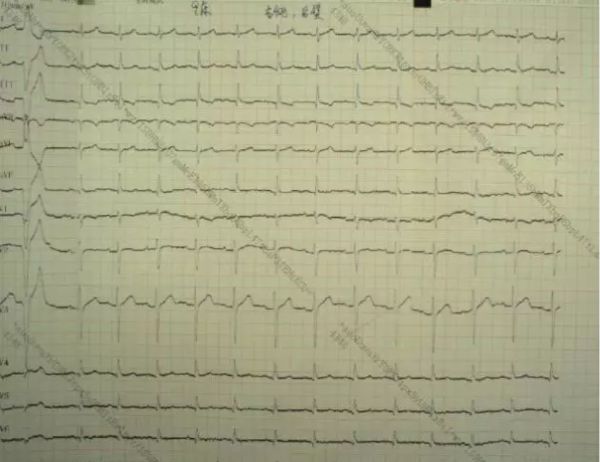
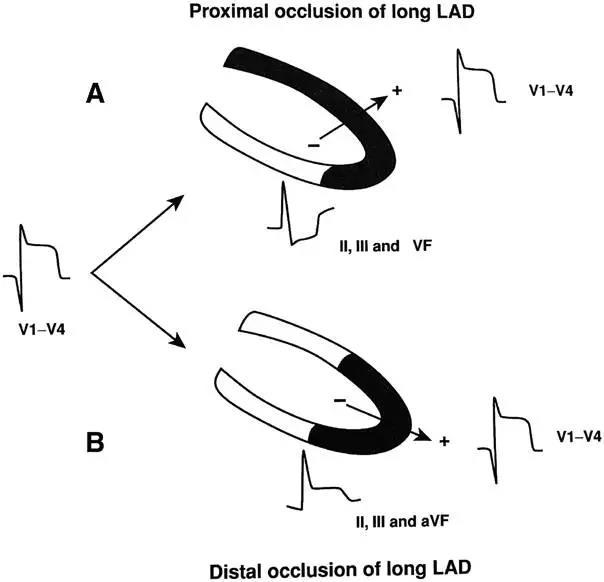
病例分享:ACS合并血小板减少症,原因分析?治疗策略?一个病例告诉你!
2017-11-07 佚名 中国医学论坛报
2016年《急性冠状动脉综合征抗栓治疗合并出血防治多学科专家共识》中明确指出:据统计,接受PCI的冠心病患者中约有6%合并血小板减少(<100×10^9/L),其出血事件发生率也明显增高。








本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











不错的文章值得推荐!
46
#ACS#
30
#血小板减少#
31
是很好的学习材料.不错.以后会多学习.
62
谢谢分享.学习了
64
学习学习学习
51
^_^^_^^_^^_^
54