PNAS:科学家发现能逆转激素耐受型哮喘的新型糖皮质激素配体药物
2019-03-28 佚名 上海药物所
徐华强课题组通过对糖皮质激素受体结构的解析,发现了糖皮质激素发挥效能的机理,并且将这一发现运用到新型高效糖皮质激素的设计上,开发了一系列新型高效糖皮质激素配体。
3月20日,中国科学院上海药物研究所徐华强课题组联合哈尔滨工业大学生命科学中心何元政课题组、美国克里夫兰临床中心布克珉(Booki Min)课题组和美国VanAndel研究所Karsten Melcher在《美国国家科学院院刊》(PNAS)上以《一种针对激素耐受型严重哮喘的新型高效糖皮质激素的研发》(Development of highly potent glucocorticoids for steroid-resistant severe asthma)为题发表了用于治疗严重型哮喘的新型高效糖皮质激素配体的研究成果。这项研究发现新型高效糖皮质激素配体在动物哮喘模型上10倍优于当前世界上临床上最有效的哮喘药物,并且首次在激素耐受型恶性哮喘的动物模型上实现了对激素抗性的扭转,为治疗致死率很高的恶性哮喘开拓了新思路。
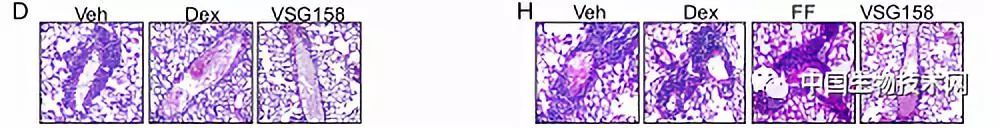
哮喘是一种常见的呼吸系统疾病,全球约有8-10%的患者。通常一般性的哮喘可以通过糖皮质激素(抗炎)和肾上腺激素受体激活剂(肺平滑肌舒张剂)联用的喷雾剂得到很好的控制。但是,严重型或恶性哮喘往往对于糖皮质激素不敏感,这就是所谓的激素抗性或激素耐受型。这种激素耐受型在所有哮喘中的致死率最高,目前尚无比较有效的治疗方法。因而,找到一种能克服肺细胞对激素的耐受性的方法是目前全世界哮喘研究的重点。徐华强课题组通过对糖皮质激素受体结构的解析,发现了糖皮质激素发挥效能的机理,并且将这一发现运用到新型高效糖皮质激素的设计上,开发了一系列新型高效糖皮质激素配体。在动物的哮喘模型上,这些高效的糖皮质激素配体表现出优于临床治疗药物的效果,特别是配体VSG158,其在动物模型上展现出到目前为止最高的抗炎效能,10倍优于临床上最有效的哮喘药物氟替卡松糠酸 (fluticasone furoate, FF)。更为重要的是,在激素耐受型的动物模型上,VSG158成功逆转动物对激素的耐受,完全抑制了肺部的各种炎症。这是到目前为止,首次利用小分子药物实现对激素耐受症状的扭转,将为治疗激素耐受型恶性哮喘开辟新的道路。
上海药物所徐华强课题组施晶晶与哈尔滨工业大学何元政、美国克里夫兰临床中心布克珉(Booki Min)课题组阮铨谭为文章的并列第一作者,徐华强、何元正和布克珉(Booki Min)为共同通讯作者。
激素敏感型Dex和VSG158都能有效抑制肺部炎症反应;严重的激素耐受型哮喘模型中Dex和现有哮喘药FF无效,但VSG158仍然有效。
原始出处:Yuanzheng He, Jingjing Shi, Quang Tam Nguyen, et al. Development of highly potent glucocorticoids for steroid-resistant severe asthma. PNAS. March 20, 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PNAS#
30
#糖皮质#
39
很好的学习机会
95
#科学家发现#
33
很好的学习机会
79
#皮质激素#
23