Am J Gastroenterol:结肠憩室会不会意味着腺瘤风险更大呢?
2016-01-24 Mechront 译 MedSci原创
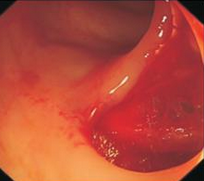
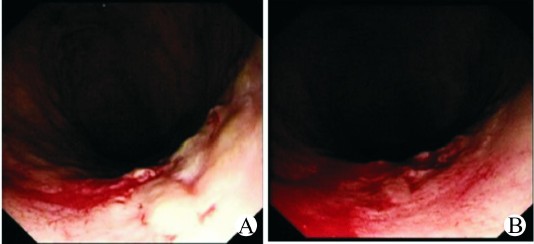
结肠镜检查常容易将漏诊的结直肠肿瘤形病变诊断为结肠憩室,那么这两者间究竟有没有什么关系呢?研究者进行了一项研究,探究结肠憩室是否会增加结肠肿瘤的风险。该研究纳入了624名行结肠镜检查的患者,获取结肠镜检查相关结果,明确结肠憩室个数以及结肠腺瘤等情况,使用Logistic回归评估校正后的OR和95%CI。纳入的患者中有216 (35%)人至少有一个结肠憩室。研究数据显示,结肠镜检查下发现的结肠憩室不
结肠镜检查常容易将漏诊的结直肠肿瘤形病变诊断为结肠憩室,那么这两者间究竟有没有什么关系呢?研究者进行了一项研究,探究结肠憩室是否会增加结肠肿瘤的风险。
该研究纳入了624名行结肠镜检查的患者,获取结肠镜检查相关结果,明确结肠憩室个数以及结肠腺瘤等情况,使用Logistic回归评估校正后的OR和95%CI。
纳入的患者中有216 (35%)人至少有一个结肠憩室。研究数据显示,结肠镜检查下发现的结肠憩室不会增加腺瘤风险 (OR 1.0, 95% CI 0.7-1.4),也不会增加晚期腺瘤风险 (OR 0.8, 95% CI 0.4-1.5)。有10个或以上结肠憩室的患者与没有结肠憩室的比较,腺瘤风险并没有增加(OR 1.1, 95% CI 0.7-1.8)。此外结肠憩室不会增加近端腺瘤风险 (OR 1.0, 95% CI 0.6-1.6),也不会增加远端腺瘤风险(OR 1.0, 95% CI 0.6-1.7)。
研究结果表明,结肠憩室不会增加患者腺瘤风险。
原始出处:
Peery AF, Martin CF,et al.Colonic Diverticula Are Not Associated With an Increased Risk of Colorectal Adenomas.Am J Gastroenterol. 2015 Dec;110(12):1694-7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#AST#
25
#Gastroenterol#
25
#GAS#
28
不错,赞一个
81
这篇文章有一定深度
112
是一篇不错的文章
79
嗯,有道理
78
#憩室#
28
hao
96