Cellectis公布了提高CAR T细胞治疗安全性和预防CRS的新方法
2019-02-26 不详 网络
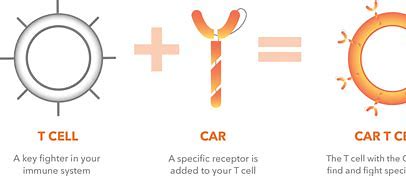
Cellectis是一家生物制药公司,专注于开发基于同种异体基因编辑的CAR T细胞(UCART)的免疫疗法,近日在《生物化学杂志》发表了一项最新研究,鉴定了由嵌合抗原受体(CAR)T细胞分泌的粒细胞巨噬细胞集落刺激因子(GMCSF)是促进细胞因子释放综合征(CRS)的关键因子,Cellectis利用这些发现来制定创新的工程策略,为开发更安全的UCART产品铺平了道路。
Cellectis是一家生物制药公司,专注于开发基于同种异体基因编辑的CAR T细胞(UCART)的免疫疗法,近日在《生物化学杂志》发表了一项最新研究,鉴定了由嵌合抗原受体(CAR)T细胞分泌的粒细胞巨噬细胞集落刺激因子(GMCSF)是促进细胞因子释放综合征(CRS)的关键因子,Cellectis利用这些发现来制定创新的工程策略,为开发更安全的UCART产品铺平了道路。Cellectis通过TALEN介导的基因失活开发了工程改造的GMCSF敲除的CAR T细胞。发现CAR T细胞中GMCSF的失活阻止了单核细胞分泌促炎细胞因子,而不损害CAR T细胞抗肿瘤的活性。
Cellectis创新项目负责人Mohit Sachdeva博士说:“CAR T细胞疗法在血液系统恶性肿瘤中达到了很高的完全缓解率,然而,这种活性药物可能显示出危及生命的炎症副作用,包括需要解决的CRS和神经毒性。我们的工程策略规避了这种有毒的副作用,并推出了更安全、且同样有效的UCART细胞,以改善患者在治疗期间的生活质量”。
原始出处:
http://www.firstwordpharma.com/node/1626814#axzz5gd5Pbuy9
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
18
#CEL#
20
#新方法#
25
#CRS#
46