辟谣|流口水是中风先兆,这说法有没有理
2017-07-04 肖蓓 澎湃新闻
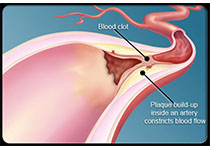
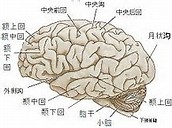
网络上流传“流口水是中风先兆”的说法,认为长年不明原因流口水,如果没有牙痛、口腔炎症等原因,首先要考虑是否为中风前兆。不少患者惊恐万分,纷纷就诊,甚至不惜做头颅核磁共振MRI检查。那么,“流口水是中风先兆”是真的吗?上海中医药大学附属曙光医院传统中医科副主任医师吴欢认为,首先,流口水的人群涉及面广,常见的有婴幼儿流口水,有老年人,也有部分中年人。其次,流口水的形式也很多,有睡觉打瞌睡位置低的一侧口
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#流口水#
39
#辟谣#
33
非常好的文章,学习了,很受益
53
学习了受益匪浅
0