PNAS:AAV2 / 9病毒疗法延迟ALS疾病发作
2019-07-06 海北 MedSci原创
超氧化物歧化酶(SOD1)的突变引起肌萎缩侧索硬化症(ALS),这是一种神经退行性疾病,其特征在于上运动神经元和下运动神经元的丧失。
超氧化物歧化酶(SOD1)的突变引起肌萎缩侧索硬化症(ALS),这是一种神经退行性疾病,其特征在于上运动神经元和下运动神经元的丧失。
已有的研究显示,过表达突变体SOD1的转基因小鼠会发生麻痹,并将错误折叠的SOD1积聚到胞内细胞器的细胞质面上,包括线粒体和内质网(ER)。
最近,人们发现,巨噬细胞移动抑制因子(MIF)直接抑制突变体SOD1的错误折叠,以及其与细胞内膜的结合。此外,完全消除内源性MIF能够加速疾病发作和晚期疾病进展,以及缩短SOD1突变小鼠的寿命,在其脊髓内也能够检测到更高量的错误折叠的SOD1。
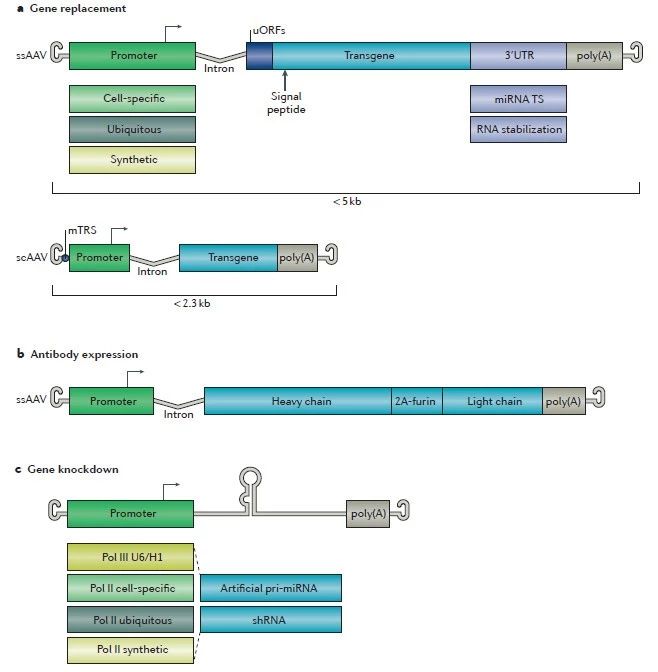
基于这些发现,研究人员使用腺相关病毒(AAV)载体在突变体SOD1G93A和loxSOD1G37R小鼠的脊髓中过表达MIF。
数据显示,注射AAV2 / 9-MIF的小鼠的脊髓中MIF mRNA和蛋白质水平增加。此外,与注射AAV2 / 9-GFP或未注射的同窝小鼠相比,注射AAV2 / 9-MIF的SOD1G93A和loxSOD1G37R突变体小鼠显示出疾病发作的显着延迟和延长的存活。
此外,在这些小鼠的脊髓中,错误折叠的SOD1的累积减少。研究人员也没有观察到MIF上调对神经胶质过度活化的影响。
因此,该研究结果表明,MIF在SOD1折叠和错误折叠机制中发挥重要作用,并强化了MIF作为体内错误折叠SOD1伴侣蛋白的假设,可能进一步暗示MIF上调调节特异性的潜在治疗作用。
原始出处:
Leyton-Jaimes MF et al. AAV2/9-mediated overexpression of MIF inhibits SOD1 misfolding, delays disease onset, and extends survival in mouse models of ALS. PNAS, 2019; doi: 10.1073/pnas.1904665116.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PNAS#
31
#AAV2#
37
#疾病发作#
35
#AAV#
31
向挑战病魔的科研人员致敬!
68