孙英贤等研究提示:血尿酸高的男士猝死风险增加,因其QTc延长
2016-12-19 卢芳 “中国循环杂志”
延长的心率校正后QT(QTc)间期是一个预测心脏猝死和心血管病死亡的重要因子。近期中国医科大学附属第一医院孙英贤等研究发现,血尿酸水平高的男性,其QTc间期延长风险增加1.4倍。换而言之,这部分人群猝死风险增高。 研究显示,随着血尿酸四分位水平的升高,不论男女其QTc间期逐渐延长。在血尿酸水平最高的四分位,在男性延长QTc间期患病率为14.8%,在女性为17.1%;而在最低四分位时,延长
延长的心率校正后QT(QTc)间期是一个预测心脏猝死和心血管病死亡的重要因子。近期中国医科大学附属第一医院孙英贤等研究发现,血尿酸水平高的男性,其QTc间期延长风险增加1.4倍。换而言之,这部分人群猝死风险增高。
研究显示,随着血尿酸四分位水平的升高,不论男女其QTc间期逐渐延长。在血尿酸水平最高的四分位,在男性延长QTc间期患病率为14.8%,在女性为17.1%;而在最低四分位时,延长QTc间期患病率在男性为11.2%,女性为13.5%。
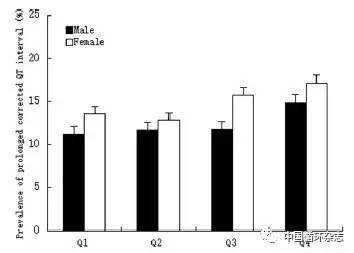
注:四分位数在男性分别为276,276~323,323~379,>379 μmol/L;在女性分别为209,209~247,247~294,>294 μmol/L
图1 不同四分位血尿酸水平男女延长的心率校正后QT间期分布状况
研究者发现,不论男女,伴有延长的QTc间期者,多年纪大,且多伴有更差的心脏代谢等相关指标;而且有心脏病史且正在用药者比例也较高;在女性则多有吸烟嗜好。
在校正多因素后,研究显示,唯有男性最高四分位水平血尿酸水平(>379 μmol /L)较最低四分位水平(≤276 μmol/L)可增加1.402倍延长QTc间期的风险。而在女性无显著相关性。
研究者推测,当血尿酸水平达到一定水平会促发炎性反应,由此进一步使得QTc间期延长;此外血尿酸参与氧化应激也是推手。
该研究共纳入辽宁农村地区11206例35岁以上受试者,男性为5104人,平均QTc间期为(422.1±24.2)ms;女性为6102人,平均QTc间期为(436.1±23.5)ms。延长的QTc间期在男性定义为≥450 ms,在女性≥460 ms。
原始出处:
Guo X, Li Z, Liu Y, et al. Sex-specific association between serum uric acid and prolonged corrected QT interval: Result from a general rural Chinese population. Medicine (Baltimore), 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血尿酸#
38
#血尿#
40
#猝死风险#
0
学习了 谢谢小编
61
是真的吗?!
68
哦!原来是这样
57