JACC:心梗后的炎性反应对大脑和心脏的功能有明显影响
2018-01-19 MedSci MedSci原创
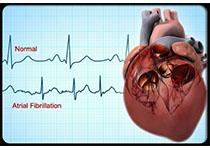
急性心梗后的局部炎性组织反应对最后的预后结果起到重要作用,全身作用引起的神经性炎症是神经退行性疾病的前兆。本研究的目的旨在通过非侵入性的正电子发射断层扫描(PET)评估心梗对心脏和大脑炎性反应的影响。本研究在对小鼠进行冠脉结扎或者假手术处理后,对所有小鼠(n=49)进行了全身线粒体转运蛋白(TSPO)的PET扫描,TSPO作为标记激活巨噬细胞和小胶质细胞的标志物,同时,急性心梗后的病人(n=3)也
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
37
#心梗后#
44
学习了谢谢分享学习!!
71
#ACC#
37