ESMO Open:TRICOLORE研究为转移性结直肠癌一线治疗提供新证据
2018-01-02 Ryy,斐斐 肿瘤资讯
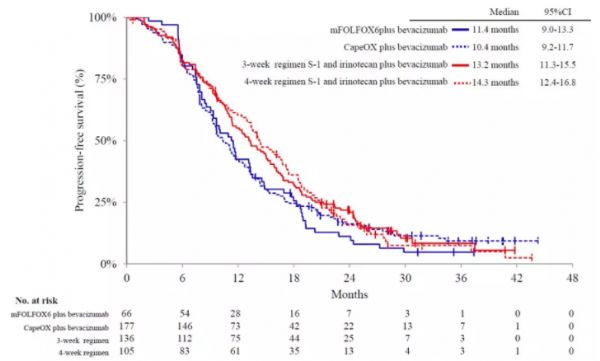
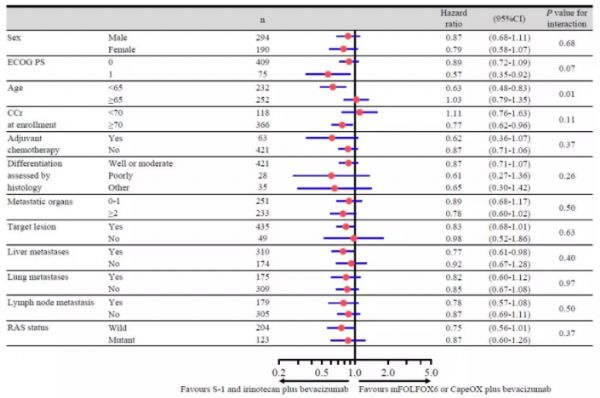
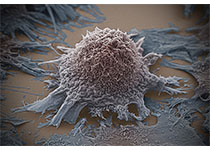
转移性结直肠癌化疗药物选择非常有限,除了FORFOX、CapeOX、FORFIRI,我们是否还能有更多选择?TRICOLORE研究(UMIN000007834)作为全球首个随机III期研究评价了口服氟尿嘧啶+伊利替康方案对于转移性结直肠癌的疗效。研究结果是否能为我们带来新的惊喜?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#SMO#
29
#PE#
30
学习了
48
学习了一下
54
学习了
60
好!很好!
66
学习!再学习!
51
再次学习
26
今天又看了一遍
28
值得学习
0