Nat Cell Biol:这个帕金森相关蛋白竟“串场”到肿瘤发生机制中!
2019-07-31 Ruthy 转化医学网
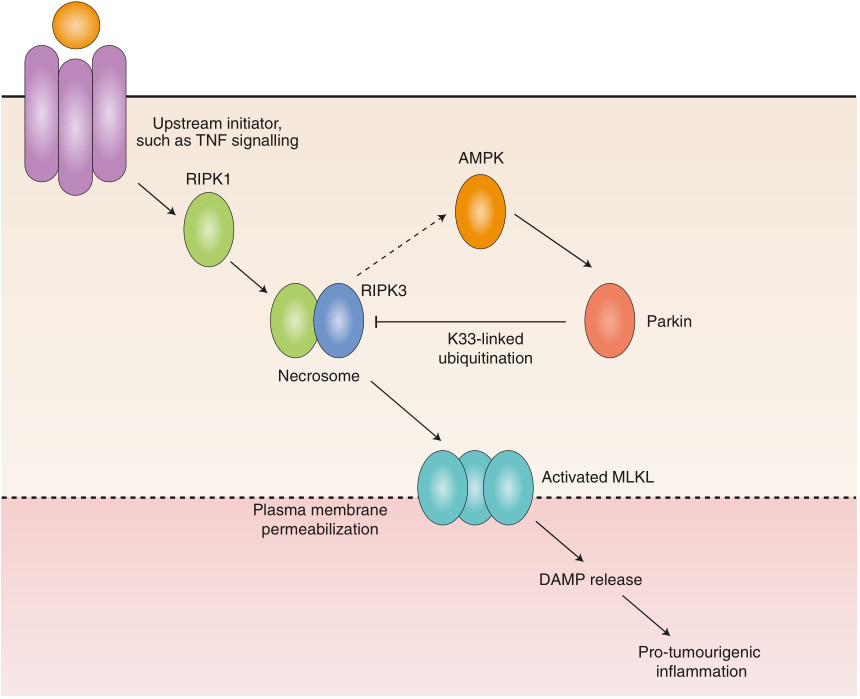
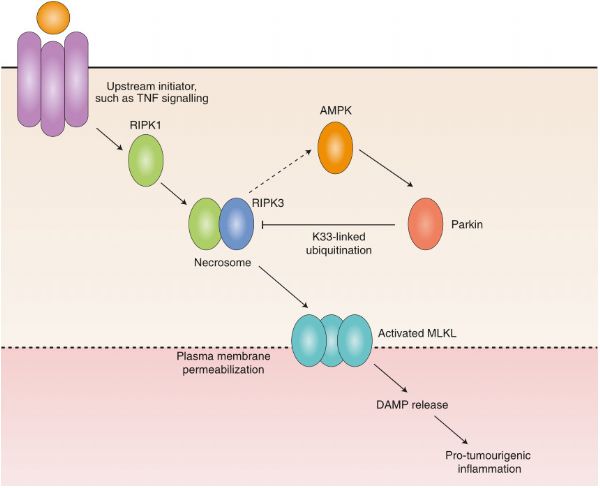
目前仍是个“谈癌色变”的时代,因为全球近1/6的死亡由癌症造成。长久以来,抗击肿瘤的征途道阻且长,虽有多项成果相继现世,但对浩浩肿瘤大军而言仍只是沧海一粟,尤其是肿瘤机制的相关研究进步缓慢。有研究显示肿瘤细胞与程序性坏死之间关系匪浅,但具体调控机制尚未明了。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
40
#Bio#
32
#Nat#
40
#Biol#
31
#Cell#
38
#肿瘤发生机制#
39
#发生机制#
37