ESC 2017:纪念冠脉介入40年 重磅研究改变临床实践
2017-08-31 佚名 医师报
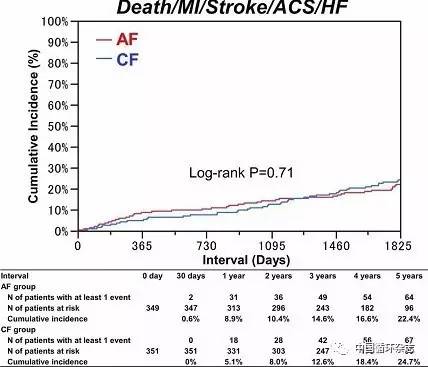
8月26~30日,欧洲心脏病学会年会(ESC 2017)在西班牙巴塞罗那召开。今年大会聚焦于“经皮冠脉介入治疗(PCI)40年”,并为此设置了特别专场,强调PCI在心血管病诊疗各方面的影响力。此外,大会发布了急性ST段抬高型心肌梗死、双联抗血小板治疗、心脏瓣膜病、外周动脉疾病4部指南。同时,CASTLE-AF、COMPASS、CANTOS等可改变临床实践的重磅研究结果也在大会中公布。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了学习了学习了学习了!
62
学习一下谢谢分享
61
#临床实践#
44
#重磅#
36
文章很好.值得分享
72
未来的发展前景广阔
55
学习了.涨知识
63
不错的.学习了.谢谢分享!
30