Cell Rep:自噬在肠道干细胞的维持和辐照诱导损伤后的再生中发挥作用。
2017-08-07 fengxiangxin MedSci原创
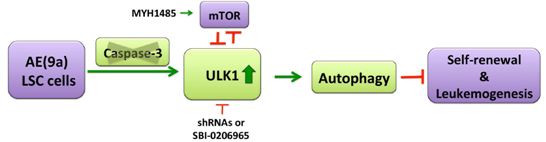
自噬是一种溶酶体降解途径,在生理平衡和很多疾病中发挥重要作用。然而,自噬在肠道干细胞(ISCs)中发挥何种作用尚不清楚。
自噬是一种溶酶体降解途径,在生理平衡和很多疾病中发挥重要作用。然而,自噬在肠道干细胞(ISCs)中发挥何种作用尚不清楚。
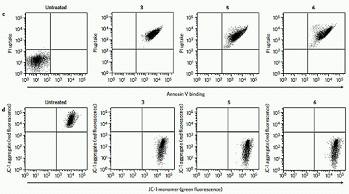
为了阐明肠道干细胞中的自噬在维持ISC平衡中是否发挥作用,研究者开展是相关实验。他们分别在Atg5ΔIEC 小鼠(Atg5fl/fl,Villin-Cre 小鼠,称Atg5ΔIEC 小鼠) 和Atg5fl/fl Ah-Cre小鼠中敲除了肠道上皮细胞 (iECs) 和除潘氏细胞外所有肠道上皮细胞( Atg5fl/fl Ah-Cre小鼠)的自噬相关基因5(ATG5),发现两个实验组小鼠的ISCs数量较对照组明显减少,并且ISC依赖的肠道恢复功能在放射刺激后受到损害。来源于Atg5ΔIEC小鼠的肠道干细胞隐窝(利氏肠腺隐窝)中活性氧水平较对照组明显升高。
另一方面,ROS诱导剂的使用降低了ISC的数量以及损害了ISC的体外再生能力,当使用抗氧化剂治疗Atg5ΔIEC小鼠之后,损伤得到恢复。
这项研究结果表明,内源性自噬通过减少过多的ROS来维持ISC的平衡。优化自噬有望将基于自噬的疗法应用于肠道损伤的治疗。
原始出处:
Asano, J., T. Sato, S. Ichinose, et al., Intrinsic Autophagy Is Required for the Maintenance of Intestinal Stem Cells and for Irradiation-Induced Intestinal Regeneration. Cell Rep, 2017. 20(5): p. 1050-1060.
本文系梅斯医学(MEDSCI)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
31
#CEL#
31
学习了谢谢分享!!
59
学习了谢谢分享!!!
79
#损伤#
27
#肠道干细胞#
30
很实用谢谢分享
66
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦
60
谢谢分享,学习了
57
不错
29