Lancet:Nivolumab为晚期胃癌或胃-食管结合部肿瘤患者带来生存获益
2017-10-15 曹守波 肿瘤资讯
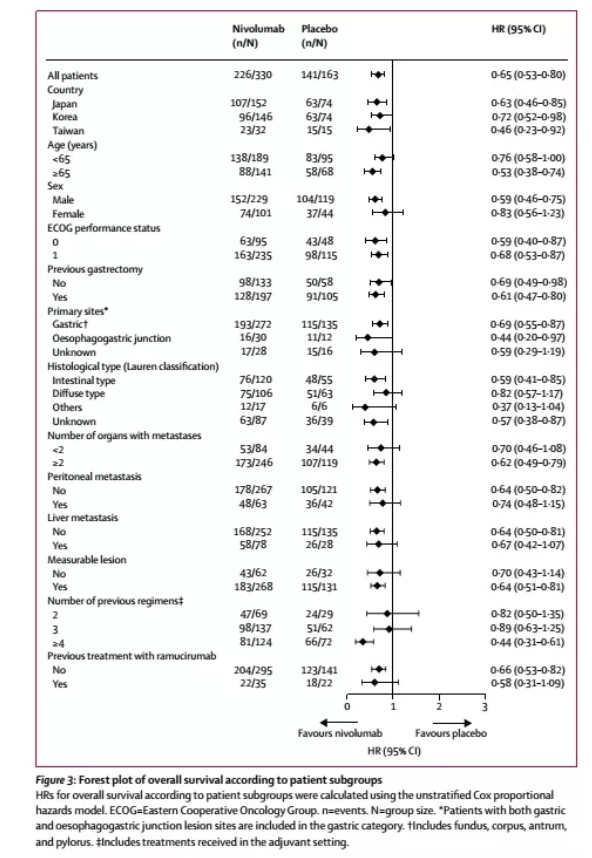
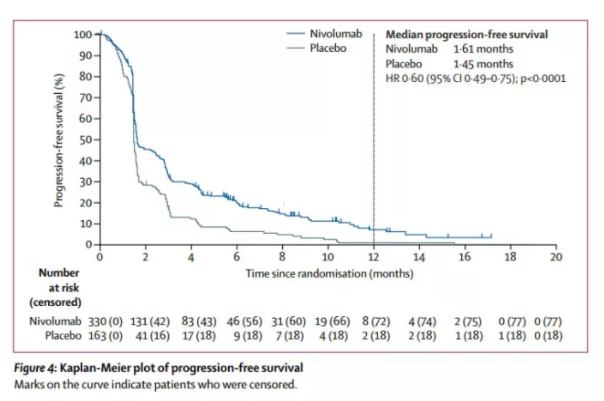
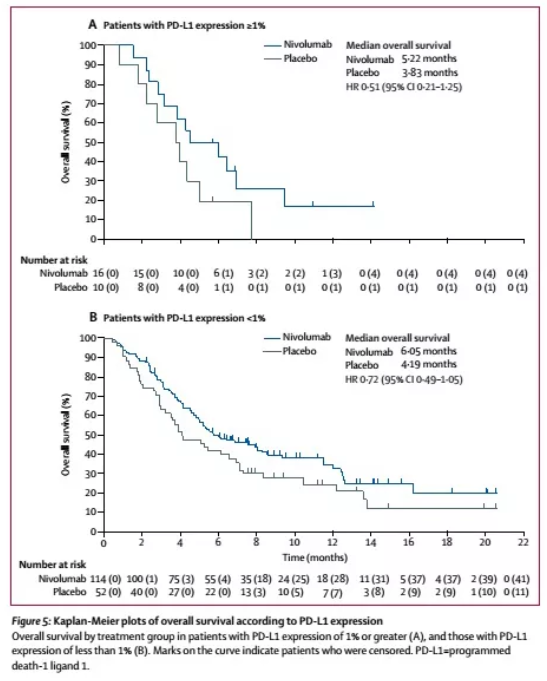
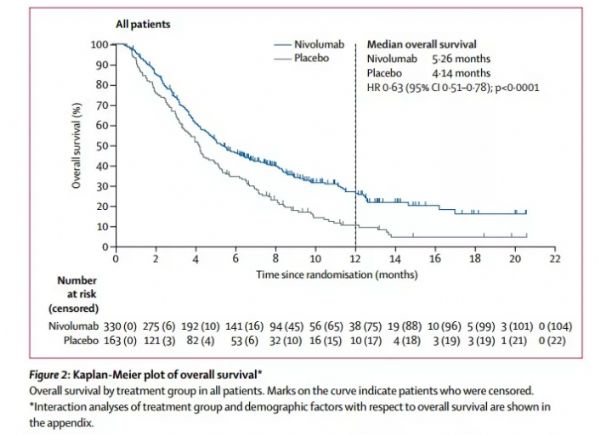
接受过两种或以上化疗方案治疗的晚期胃癌或胃-食管结合部肿瘤患者通常预后欠佳,并且对于这一部分患者,目前指南并没有特殊推荐某一种治疗方式。Nivolumab是PD-1的单克隆抗体抑制剂,本项研究旨在评价nivolumab对之前接受过两种或以上化疗方案治疗的晚期胃癌或胃-食管结合部肿瘤的有效性和安全性,相关研究成果发表在Lancet。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#mAb#
35
#生存获益#
35
#NIV#
33
#Lancet#
30
#晚期胃癌#
34
#肿瘤患者#
24
#食管#
27
学习啦!谢谢分享!
66
学习了.谢谢
63