15例应激性心肌病诊治经验:11例ST段抬高,一例80岁老人生气后再犯
2019-06-23 卢芳 中国循环杂志
应激性心肌病,最初被日本学者所描述,对于国人,都有哪些特点?阜外医院张峻、罗晓亮等对阜外医院确诊的15例应激性心肌病进行了总结:应激性心肌病患者常有超声心动图节段性室壁运动异常及室壁瘤样改变,伴有NT-proBNP明显增高。
研究发现,应激性心肌病发病初期NT-proBNP水平明显增高,经系统治疗后可明显下降,变化较同期心肌梗死患者更显着。
15例患者中,11例患者表现为一过性ST段抬高,继之出现T波倒置,4例患者表现为一过性ST段压低伴T波倒置。
作者称,应激性心肌病患者发作初期多伴有心电图异常,通常与急性ST段抬高型心肌梗死中所见相似,不同之处是很难根据心电图改变定位犯罪血管,ST段抬高常见,最常出现在胸前导联,V5、V6导联易受累,这与该研究一致,本研究中仅有一例患者为肢体导联单独受累。
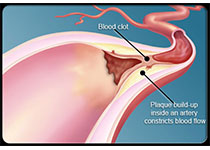
14例患者行冠状动脉造影检查,1例患者发现前降支冠脉肌桥,收缩期压缩50%,4例患者冠脉造影未见狭窄,9例患者发现冠状动脉粥样斑块形成,狭窄程度<50%。9例同期行左心室造影,发现有心尖部球形样变。
不过,鉴于其中1例患者2年后争吵复发再次住院,研究者建议要注意出院前宣教,警惕复发。
这项研究共分析了15例应激性心肌病患者,其中女性居多为13例。入院时,患者平均左心室射血分数为44.8%,NT-proBNP平均为2429.10 pg/ml。
在入院治疗后,平均左心室射血分数提升为62.9%,NT-proBNP平均为715.14 pg/ml。
值得注意的是,一项发表在Ciruclation上的研究显示,应激性心肌病长期预后差,持续存在亚临床心肌功能障碍相关的症状和心功能损害。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#应激性心肌病#
42
#诊治经验#
32
#ST段抬高#
42
#应激#
28
#肌病#
38
#ST段#
37