这项研究目的是使用植入后计算机体层摄影(CT)评估经导管主动脉瓣置换术(TAVR)后不良冠脉通路的发生率。
目前很少有关于使用植入后CT评估TAVR后冠脉通路的真实数据。
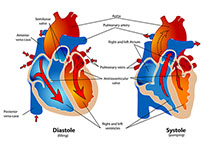
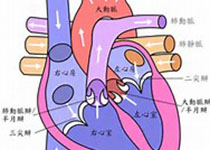
对66例Evolut R或Evolut PRO瓣膜患者和345例SAPIEN 3瓣膜患者的TAVR后CT进行了分析。评估从经导管心脏瓣膜(THV)入口到冠脉口的距离以及THV连合与冠脉口之间的重叠。如果冠脉口位于裙部下方或每个冠脉里THV连合前方在裙部上方,则冠脉通路被定义为不良通路。
在Evolut R/Evolut PRO组中,34.8%的左冠脉(n=23)和25.8%的右冠脉(n=17)观察到CT识别的不良冠脉通路特征,而在SAPIEN 3组中,左冠脉的百分比为15.7%(n=54),右冠脉为8.1%(n=28)。在Evolut R/Evolut PRO组中,TAVR后进行了16例冠脉介入治疗,而SAPIEN 3组中TAVR后进行了64例冠脉介入治疗。在介入水平的分析中,Evolut R/Evolut PRO组(0.0%vs.77.8%;p=0.003)和SAPIEN 3组(33.3%vs.91.4%;p=0.003)CT识别出不良冠脉通路患者的选择性冠脉介入成功率均明显低于冠脉通路良好的患者。
相当大比例的患者在TAVR后难以接受冠脉介入治疗。裙边或连合高度低的THVs和用于实现与天然主动脉瓣连合对齐的大开孔设计有利于将来的冠脉介入。(经导管和外科主动脉生物瓣血栓形成的评估及其抗凝治疗[RESOLVE];NCT02318342)
原始出处:
Tomoki Ochiai. Coronary Access After TAVR. JACC:Cardiovascular Interventions. 23 March 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











点赞👍
48
#JACC#
34
#AVR#
38
#ACC#
27