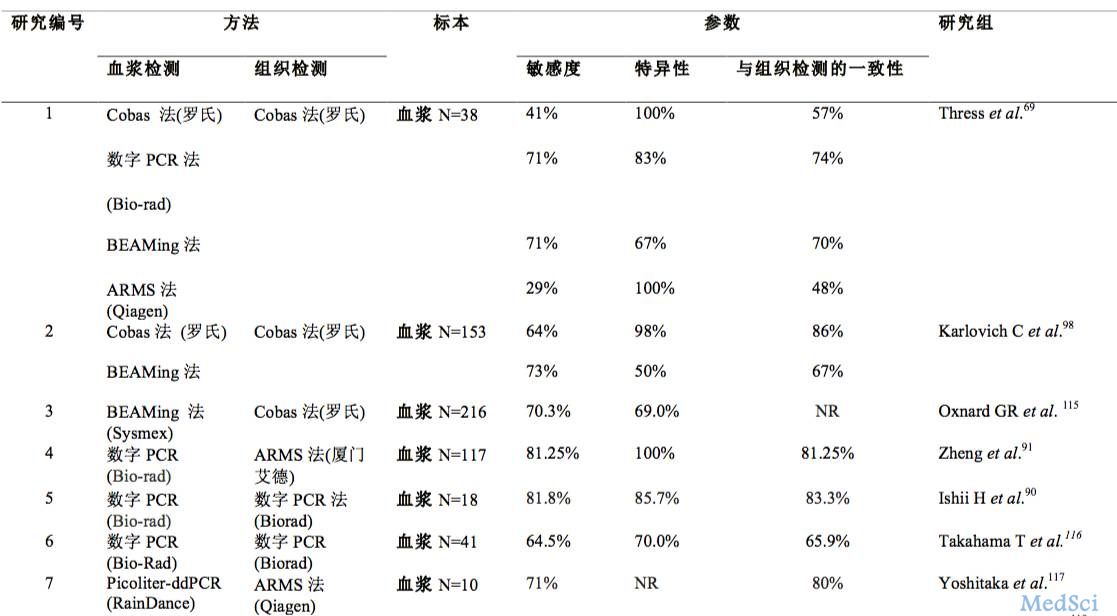
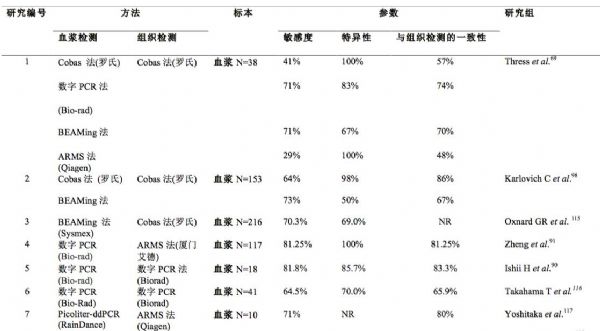
EGFR-TKI耐药后的检测标本选择:组织活检vs.液体活检
2017-08-09 佚名 肿瘤资讯
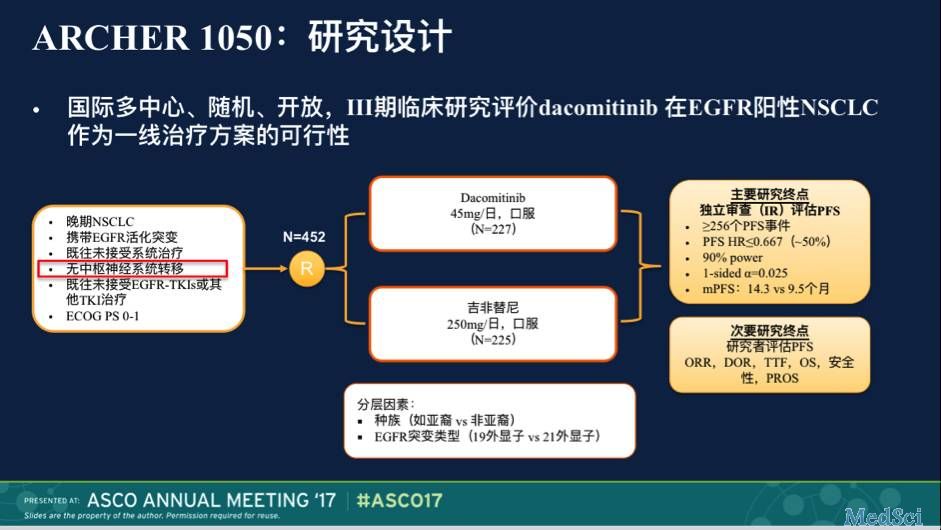
奥希替尼是一种不可逆的三代EGFR-TKI,可以选择性地抑制EGFR敏感突变和T790M耐药突变。2017年3月,奥希替尼在华上市,开创了EGFR TKI耐药后T790M阳性患者的精准治疗新时代。随着泰瑞沙的上市,如何敏感、准确地检测T790M突变成为临床关注的热点。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#标本#
58
学习了,谢谢分享
65
#活检#
34
#EGFR-TKI#
48
#TKI#
43
#GFR#
33
#组织活检#
39
该研究结果很好,指导临床实践很有价值
54
谢谢分享,学习了
56
学习了谢谢分享
52