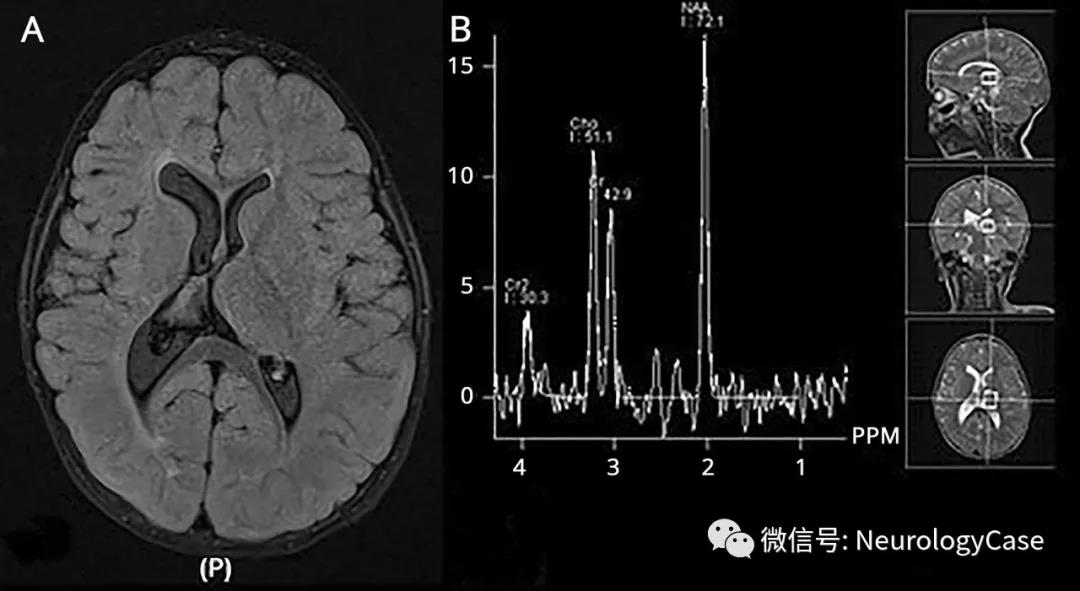
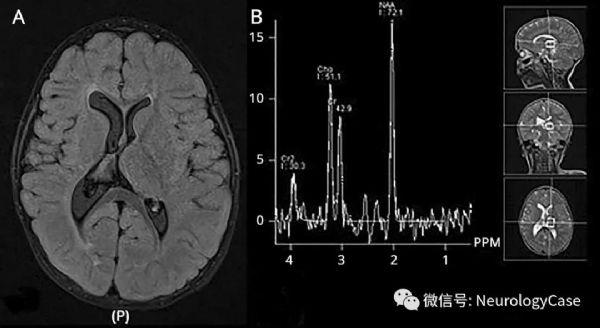
Neurology:病例:孤立的半侧丘脑过度发育
2018-08-18 zyx整理 神经科病例撷英拾粹
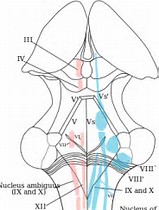
17月大的男孩,表现为左侧轻偏瘫,没有其他任何神经功能障碍。脑MRI提示左侧丘脑明显肥大。使用对比剂前后右侧丘脑信号无殊,未见FLAIR高信号或弥散受限病灶。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Neurol#
15
了解一下
46
#发育#
15
#丘脑#
19
#丘脑#
24