中国NMPA批准ZEJULA(Niraparib)用于复发性卵巢癌患者的维持治疗
2019-12-28 Allan MedSci原创
Zai Lab生物制药公司近日宣布,中国国家药品监督管理局(NMPA)批准了ZEJULA(Niraparib)的新药申请(NDA)用于对铂类化学疗法有完全或部分反应的复发性上皮性卵巢癌、输卵管癌或原发性腹膜癌患者的维持治疗。
Zai Lab生物制药公司近日宣布,中国国家药品监督管理局(NMPA)批准了ZEJULA(Niraparib)的新药申请(NDA)用于对铂类化学疗法有完全或部分反应的复发性上皮性卵巢癌、输卵管癌或原发性腹膜癌患者的维持治疗。ZEJULA是一种有效且具有高度选择性的PARP1/2抑制剂,在给药前无需进行BRCA突变或其他生物标记物的测试。
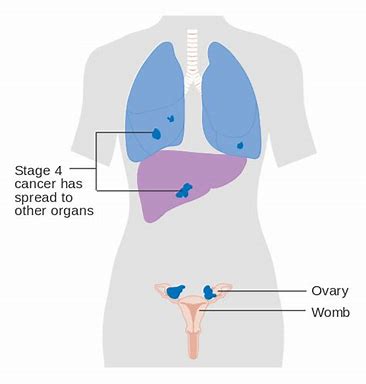
Zai Lab创始人兼首席执行官Samantha Du博士表示:“ZEJULA是我们在中国大陆首个获得NMPA批准的产品”。卵巢癌是卵巢肿瘤的一种恶性肿瘤,是指生长在卵巢上的恶性肿瘤,其中90%~95%为卵巢原发性的癌,另外5%~10%为其它部位原发的癌转移到卵巢。
原始出处:
https://www.firstwordpharma.com/node/1690167
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Zejula#
31
#复发性#
32
#APA#
0
#复发性卵巢癌#
25
#Niraparib#
26