CSCO2017·现场:拨云见日,肿瘤相关性贫血呼唤规范诊疗
2017-09-29 毕雪立 医师报
9月27-30日,CSCO2017盛大开幕。CSCO历来重视肿瘤相关性贫血的规范治疗,于2012年正式发布了《肿瘤相关性贫血临床实践指南》,后于2013年、2015年分别作了更新。除此之外,CSCO于年会期间设置“肿瘤相关性贫血论坛”,邀请在此领域顶级专家学者进行学术分享。
9月27-30日,CSCO2017盛大开幕。CSCO历来重视肿瘤相关性贫血的规范治疗,于2012年正式发布了《肿瘤相关性贫血临床实践指南》,后于2013年、2015年分别作了更新。除此之外,CSCO于年会期间设置“肿瘤相关性贫血论坛”,邀请在此领域顶级专家学者进行学术分享。
由马军教授、王杰军教授和姚阳教授担任论坛主席,邀请沈志祥教授、姚阳教授、宋正波教授以及王健民教授,对肿瘤相关性贫血的相关内容,进行了精彩纷呈的学术讲座。现摘录各位专家对促红细胞生成素(EPO)和铁剂治疗贫血的精彩内容,分享如下,以飨读者。
中国贫血发病率高 治疗率低
贫血是指外周血中单位容积内红细胞数减少或血红蛋白浓度减低,致使机体不能对周围组织细胞充分供氧的疾病。肿瘤相关性贫血是指肿瘤患者在其疾病发展过程中,以及治疗过程发生的贫血。
上海交通大学医学院附属瑞金医院沈志祥教授指出,欧洲肿瘤患者的贫血发病率为63.4%,而我国2012年数据显示,发病率与之相近,高达60.83%。但是,中欧之间贫血的治疗率相差甚远,欧洲接受治疗者高达38.9%,而我国仅为6.9%。
“研究发现,我国轻度贫血患者中只有不到2成得到治疗,而对于极重度贫血患者,按指南规定应全部接受治疗,但临床上仅1/2患者得到治疗,且治疗效果并不尽如人意。”上海长海医院王健民教授强调,中重度贫血治疗率过低,未达到早治疗,规范治疗的标准,我国对肿瘤相关性贫血的治疗远远不足,对其重视程度亟待提高。

图1 中欧肿瘤相关性贫血治疗率对比
贫血危害生活质量与加重病情
“贫血的高发病率与低治疗率,已经严重影响我国居民的生活质量。” 沈志祥教授指出,贫血影响患儿睡眠质量,进而对其生长发育产生负面影响,另外,贫血还严重制约全身各系统的正常运转,心血管、呼吸、泌尿生殖等系统皆深受其害。沈志祥教授认为,贫血可能与肿瘤的发生相关,需要进一步验证。
四位专家不约而同的提及贫血对患者生活质量不良影响,王健民教授强调,贫血的严重程度与生活质量直线相关,贫血越严重,生活质量越低。
另外,“贫血导致组织乏氧,降低了组织细胞对肿瘤药物及放疗等的敏感性,影响了肿瘤治疗的临床疗效。”上海长征医院王杰军教授指出。因此,对于肿瘤相关性贫血的患者,必须及时纠正缺氧状态,以提高临床疗效。
“在临床中,很多‘生无可恋’的肿瘤患者,都是贫血导致”,上海市第六人民医院姚阳教授建议,积极改善患者贫血状态,正确处理生命、性命、生活三者的关系,将患者性命变成生命,让他的生活更有质量。姚阳教授倡议,医生在治疗肿瘤这种“大病”的时候,不能忽视患者的“小问题”,如头昏,贫血等,因为这些小问题直接关系到患者的生活质量。医生多一分人文关怀,患者多一分生活质量。
废用之争的“缘起缘灭”
对于EPO可否应用于肿瘤相关性贫血,可谓几经波折。其废用之争起源于Lancet上发表的一篇荟萃分析,其结论是促红细胞生成素类药物(ESAs)缩短了患者的总体生存时间、无进展生存时间以及可促进肿瘤进展。此文章一出,许多肿瘤医生对ESAs产生了质疑,在使用时顾虑重重。ESAs的“事业线”似乎陷入“低谷”。
但是,上帝给ESAs关上一扇窗,却又为它打开了一扇门。另一项JCO荟萃分析研究得出了与之完全相反的结论,即ESAs不会增加死亡率,也不会对无进展生存时间和疾病进展产生影响。这无异于扫走雾霾,曙光重现。
“理智的医师最善于分析理论与实践关系”,姚阳教授对两篇荟萃分析做了对比。他指出,从研究对象看,Lancet荟萃分析纳入多个超适应症使用ESAs的研究,如针对放疗或者不进行化疗和放疗的患者,而JCO研究只在适应症规定的化疗研究之内。其次在试验设计合理性上,Lancet荟萃分析纳入的研究在安慰剂对照,随机抽样步骤方面均不如JCO荟萃分析定义明确。最后,从终点事件上分析, Lancet荟萃分析的研究终点定义不如JCO荟萃分析清晰。
“有经验的医师最善于解决治疗过程中利与弊的关系。”姚阳教授总结道,以上3点表明,JCO荟萃分析是更符合临床实践,更具有临床指导意义的分析。
“为什么乳腺癌患者用EPO降低存活时间?”王杰军教授进一步介绍,EPO应用最早开始于放疗,因为放疗降低了组织的敏感性。放疗科医生使用EPO来升高组织氧含量,以此提高放疗的敏感性。但是,他们使用EPO升血红蛋白时,“用力过猛”将之从正常值升至过量值,这就出现了EPO升高乳腺癌患者死亡率的问题。所以,王杰军教授强调,在EPO治疗贫血时,应注意规范治疗。
指南推荐EPO 应规范应用
目前,临床上对肿瘤相关性贫血常用的手段包括输血、EPO治疗和铁剂治疗。中国临床肿瘤学会发布的肿瘤相关性贫血临床实践指南(2015-2016版)中推荐EPO(如益比奥等)治疗化疗相关性贫血的Hb初始值≤100 g/L,其目标值为110~120 g/L;如果超过120 g/L,则需要根据患者个体情况减量或停用。指南强调,原则上,Hb<80 g/L时,不建议进行化疗。沈教授强调,在治疗贫血时,首选考虑EPO或EPO+补铁治疗,不应首选输血治疗。
“EPO治疗作为CRA常用的治疗方法,不仅能减少因贫血而导致的输血需求,还能提高患者的生存质量,更加符合患者的生理状况。”浙江省肿瘤医院宋正波教授强调,在最新的荟萃分析中指出,在说明书用法之内使用ESAs是安全的,最重要的是,ESAs 和患者的 OS、PFS、肿瘤进展无任何相关性。
提及EPO的临床应用,就不能忽视EPO-ANE-3010研究。它是近年来关于ESAs使用于乳腺癌合并贫血患者的规模最大,时间跨度最长的前瞻性研究。该研究从2006年开始,直至2014年的数据发布,耗时8年纳入19个国家,2098名乳腺癌患者。研究发现,似乎有个别患者在使用了Epoetin Alfa治疗贫血后,有加速肿瘤生长的迹象。但从统计分析上来看,不具有显着的统计学差别。
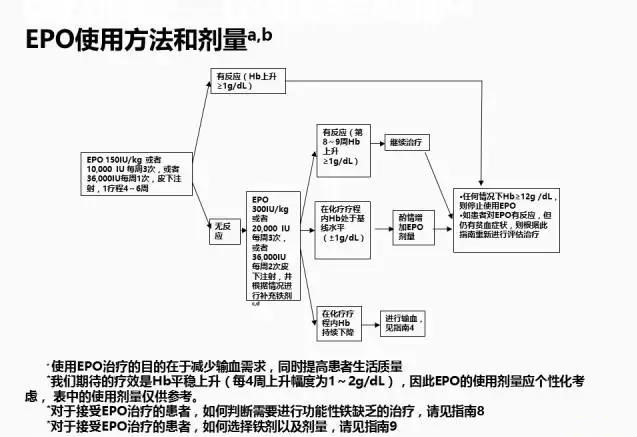
图2 指南中EPO使用方法和剂量
“经过18年的探索,我们现在知道EPO的使用频率、使用量,进而搞清楚它与血栓及OS的关系。”哈尔滨血液病肿瘤研究所马军教授进一步指出,现在肿瘤科医生可以很好的把握EPO的用法用量,进行个体化规范化治疗。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#规范诊疗#
50
#相关性#
40
学习一下谢谢分享
59
谢谢了.学习
63
厉害了我的哥
70
学习.谢谢分享
62