Arthritis Rheumatol:NLRP3中低外显率变体的临床和分子表型
2017-07-18 xiangting MedSci原创
低外显率NLRP3变体患者表现出明显的临床表型和包括IL-1β和非IL-1β介导的炎症通路活化的中间生物表型。
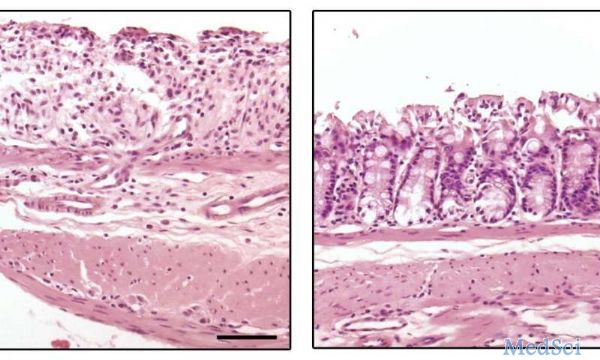
Cryopyrin相关性周期综合征(CAPS)是由NLRP3基因获得性功能突变引起的,可导致白介素-1β(IL-1β)过度释放和全身炎症。虽然致病性NLRP3变体表型已被很好地描述,但是低外显率NLRP3变体代表了重要的临床挑战。这项研究的目的是确定低外显率NLRP3变体患者的临床表型、体外生物表型和抗IL-1治疗的效果。
2012年5月至2013年5月间在7个中心入组有症状的低外显率NLRP3变体患者。对照组是有已知致病性NLRP3变体的患者。记录临床表现和CAPS炎症标记物。进行包括半胱天冬酶-1活性,NF-κB释放,细胞死亡和IL-1β释放的炎性体激活的功能测定。评价IL-1的治疗效果。进行低外显率和致病性NLRP3变体间的比较。
研究包括45例患者,21例为女性(47%); 26/45(58%)为儿童。NLRP3低外显率变体:Q703K(n = 19),R488K(n = 6)和V198M(n = 20)。对照组:28例为致病性NLRP3变体。低外显率NLRP3变体患者发热次数(76%)和胃肠道症状(73%)明显更多;眼病,听力丧失和肾脏受累较少见。与野生型和致病性NLRP3变体相比,功能性炎症试验发现了低外显率NLRP3变体中的中间表型。所有接受治疗患者均对IL-1抑制剂有反应,50%的患者有完全反应。
低外显率NLRP3变体患者表现出明显的临床表型和包括IL-1β和非IL-1β介导的炎症通路活化的中间生物表型。
原始出处:
JB Kuemmerle-Deschner,et al. Clinical and molecular phenotypes of low-penetrance variants in NLRP3: Diagnostic and therapeutic challenges. Arthritis Rheumatol.10 July 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Arthritis#
31
#ART#
27
#NLR#
53
#表型#
40
#NLRP3#
51