经腹膜外联合会阴完整切除侵袭性血管黏液瘤 1 例
2019-11-08 马骁 王涛 商晓 实用妇产科杂志
患者, 32 岁,因外阴肿物进行性增大 5 年,于 2018 年 3 月 9 日入我院。患者5 年前扪及左侧外阴一直径约1 cm 肿物,质 软,界清。2014 年7 月中旬肿物增大至直径3 cm 左右,患者遂 就诊于当地医院,当地医院考虑“左侧尿生殖膈缺损并疝形 成”,遂行左侧尿生殖膈缺损并疝修补术。3 年前再次发现左 侧外阴肿物,且于妊娠期间增大明显,偶有胀痛,于腹压增大、 经期时痛感明显,有便
1 病例报告
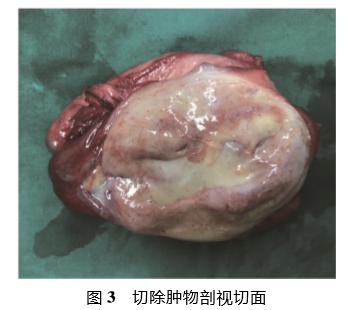
患者, 32 岁,因外阴肿物进行性增大 5 年,于 2018 年 3 月 9 日入我院。患者5 年前扪及左侧外阴一直径约1 cm 肿物,质 软,界清。2014 年7 月中旬肿物增大至直径3 cm 左右,患者遂 就诊于当地医院,当地医院考虑“左侧尿生殖膈缺损并疝形 成”,遂行左侧尿生殖膈缺损并疝修补术。3 年前再次发现左 侧外阴肿物,且于妊娠期间增大明显,偶有胀痛,于腹压增大、 经期时痛感明显,有便秘, 3~7 天/次,大便干结,小便无异常。 因左侧外阴肿物逐渐增大,患者遂于 2018 年 1 月 12 日就诊于 外院,行妇科 B 超检查提示:膀胱后方与子宫左侧间见混合回 声,约 6. 4 cm×3. 3 cm×3. 7 cm,回声不均,界欠清,与左侧会阴 区肿物相连,腹压增加时可见上述混合回声滑动,最窄处约 1. 9 cm,考虑为盆腔肿物合并疝( 盆底疝) 。CT 检查:膀胱及尿 道、阴道左侧、左侧闭孔内肌右侧异常密度影,最大截面为 8. 7 cm×5. 1 cm,肿物性质待查。MRI 检查: 子宫及膀胱左侧可见 8. 1 cm×5. 1 cm×11. 1 cm 软组织肿块,沿尿生殖膈延伸至左侧 大阴唇区,病灶内信号不均匀,可见分层状及漩涡状改变,增强 扫描呈较明显不均匀强化,病灶局部与闭孔内肌分界不清楚。 为进一步诊治, 2018 年 3 月 7 日患者前来我院就诊,门诊考虑 侵袭性血管黏液瘤( aggressive angiomyxoma, AAM) 可能, 2018 年 3 月 9 日收入我院。既往史: G1P1, 2015 年因“巨大儿”足月 行剖宫产娩一活男婴,“头孢他啶”皮试阳性,余无特殊。 入院后查体:一般情况好,耻骨联合上可见约 10 cm 陈旧 性剖宫产横切口,余未见特殊。妇科检查:左侧大阴唇肿大,表 面可见血管,可扪及约 8 cm×7 cm 肿物( 见图 1) ,界尚清,质 软,活动,无压痛;子宫左前方可扪及大小约 4 cm×3 cm 肿物, 界尚清,质软,活动欠佳。我院查肿瘤标志物均( -) 。术前诊 断:盆底肿物:侵袭性血管黏液瘤? 剖宫产史;左侧尿生殖膈缺 损并疝修补术史。于 2018 年 3 月 13 日行腹膜外入路联合会 阴路径肿物切除术。术前请泌尿外科会诊,放置双侧输尿管 DJ 管,充足备血。MRI 检查提示肿物未穿透腹膜,位于腹膜 外,肿块形态不规则,沿尿生殖膈延伸至左侧大阴唇区,最窄处 于耻尾肌、盆底筋膜与耻骨联合之间,病灶内信号不均匀,可见 分层状及漩涡状改变。结合盆腔解剖结构,采用腹膜外入路联 合会阴路径行肿物切除术,术中见耻骨后膀胱左侧大小约 12 cm×4 cm 肿物,质韧,周边有多层膜状包膜,最窄处于耻尾 肌、盆底筋膜与耻骨联合之间,粘连于盆膈,与 MRI 检查表现 一致( 见图 2) 。肿物穿过盆膈直达会阴部并向外突出,突出部 分约 7 cm×5 cm。术中主要利用手指触觉,了解、确定肿物生 长方向及界限,沿侵袭间隙探查,将肿物与周围组织钝性分离,但自盆膈向下分离困难且间隙狭窄不清,遂在左侧大阴唇肿物 突出处作一约 4 cm 纵切口,钝性向上分离,贯通盆膈游离肿 物,完整切除肿物送病理,手术顺利,术毕放置腹膜外引流管 1 根。肿物大体观:形态不规则,呈树突状,约 25 cm×5 cm,边界 较清,质韧;剖视切面:呈灰白、灰红和灰黄色,黏液胶冻状,可 见细小出血点( 见图 3) 。术后病理报告: 病变符合 AAM。术 中无实质脏器损伤,出血少。术后患者恢复好,予以硫酸镁湿 敷缓解外阴水肿,术后第 3 天腹膜外引流量仅 5 ml 遂拔除引 流管,术后第 7 天拔除 DJ 管,术后第 8 天好转出院。术后 3 个月于我院门诊复查,查体:未见大小阴唇肿大,未扪及明显肿 物样突起;阴道内及盆腔内未触及明显肿物。盆腔 MRI 检查: 盆底肿物切除术后改变,未见明显肿物。该患者随访至今尚未 见复发。

2 讨 论
AAM 于 1983 年首次被 Steeper 等报道[1],它是一种来源 于间叶组织的软组织肿瘤,呈低度恶性潜能。多见于生育年龄 女性,好发盆腔、会阴等区域。但发病机制及好发于上述区域 的原因尚无结论。AAM 呈侵袭性生长,多与周边组织界限不 清,其治疗多采用阴式或经腹入腹腔手术切除肿瘤,但多不能 完整切除,术后易复发。
2.1 术前评估 AAM原发部位多较深,缺乏特异性症状及体征, 难以在疾病早期发现,多因突出于外阴或会阴被发现,发现时多大 于10 cm[2],误诊率可高达70%~100%[3],诊断依靠病理及免疫组 化结果。通常AAM 在 B 超检查多表现为边界较清,形态不规则 的低回声区;CT检查则多表现为低密度或肌肉等密度的囊实性占 位;增强MRI 检查可出现“漩涡状”或“层状”特征性改变[2, 4 ] 。与 B超、 CT相比, MRI 检查对诊断及治疗 AAM 具有更重要的意义: 用于术前评估肿瘤大小、侵袭程度、与周围组织关系;根据肿瘤生 长延伸情况,选择最佳手术方式,起术中指示作用;用于评估 AAM 对激素治疗反应及了解术后残余灶和肿瘤复发情况。 在本院就诊前,该患者相继被误诊为左侧尿生殖膈缺损并 疝形成、盆腔肿物合并盆底疝。但该患者为慢性病程,无腹压 突然增大等诱因,随着肿物增大偶有胀痛、便秘,但无下坠感、 大小便失禁等。MRI 等影像学检查提示盆腔内可见一约 8~11 cm 不规则形态肿物,且该肿物与左侧大阴唇肿物相连。但盆 底疝、盆膈疝极少合并盆腔肿物,且患者在当地医院术后 1 年 内肿物再次出现并增大。因此,我院术前考虑诊断为外阴、盆 腔肿物侵袭性血管黏液瘤可能。
2. 2 手术治疗 目前,手术治疗仍然是 AAM 的一线治疗方 法。激素治疗、放化疗等方法亦有尝试,但有效性有待进一步 确证。手术方式由肿瘤位置、大小、侵袭程度以及是否合并其 他疾病决定。其关键是尽可能将肿瘤完整地与周围组织器官 分离和切除。大多数文献报道认为完整切除肿瘤可减少术后 复发率,因此提倡在保证生殖道、盆腔器官解剖和功能的前提 下,尽可能完整地切除肿瘤,恢复周围组织器官解剖和功能;对 于位置深、与周围组织关系致密的 AAM,若完整切除手术损伤 大,允许部分切除肿物。本例患者术前进行了充足备血和术前 准备,综合应用 MRI 等辅助检查进行指示引导,术中未损伤周 围实质脏器,出血量少,术毕放置腹膜外引流,术后第 3 天腹膜 外引流量仅为 10 ml,拔除引流管,进一步说明术中完整地沿肿 物边界分离切除肿物,并未形成大的手术创面。 据文献报道[4],阴式肿物切除术多适合发现较早、体积小, 局限于会阴、阴道的 AAM。经腹或经腹联合阴式肿物切除术适于生长广泛、巨大的 AAM。对于超过盆膈延伸至体表的 AAM,不建议行腹腔镜下肿物切除术,腔镜手术缺乏触觉,无法 充分探查,术中分离深度和手术范围有限,且腔镜下不易止血, 完整切除和取出盆腔 AAM 困难,故建议行开腹手术。本病例 根据 MRI 检查提示的肿瘤位置及大小,采取经腹膜外入路联 合会阴路径完整切除盆腔 AAM,并未入腹腔,此种术式国内外 鲜见报道。术中通过术者的触觉钝性分离肿瘤与周围组织,沿 侵袭间隙顺利探查至肿物穿过盆膈处,完整切除了盆腔和外阴 AAM,术中无脏器损伤,出血少,无锐性分离的肿瘤创面。 尽管本病例采取经腹膜外入路联合会阴路径术中出血少、 未 损伤周围重要脏器,但既往有 AAM 经腹或阴式手术中出血多、 肿 瘤巨大、生长广泛,与周围脏器关系密切,造成膀胱、直肠等手术损 伤的文献报道。因此仍建议无论采取何种术式,均应做好术前准 备,术前多科会诊(泌尿外科、肛肠外科、整形外科等),必要时放置 DJ 管;密切结合影像学辅助检查结果,了解肿瘤位置、大小及延伸 方向,明确与周围组织器官关系,选择合适的术式及入路。如肿瘤 较大并且“跨盆膈”生长,尽量避免腔镜手术。因部分 AAM 与周 围组织边界不清晰且本身富含血供,术中应充分利用手指触觉, 沿 组织间隙探查、操作,尽可能减少锐性分离、切割,以缩小手术创 面、减少出血与手术损伤。术毕可放置引流管,监测创面出血情 况。术后予以硫酸镁湿敷减轻外阴水肿等。
2. 3 预后 若误诊或长时间未诊断都将导致不恰当的治疗, 影响疾病预后[5]。AAM 术后复发率在 30% ~ 72%之间,最短 在术后 2 个月复发[6],最长为术后 20 年[7]。
综上所述,如患者因会阴/外阴部无痛肿块就诊,应考虑到 AAM可能性,完善腹部或盆腔影像学检查,以助诊断及术式选择。 手术是AAM一线治疗方案,经腹膜外联合经会阴完整切除盆腔 AAM,术者可充分利用触觉探查, 将AAM与周围组织钝性分离, 不 入腹腔,减少盆腔粘连发生,对患者损伤小、出血少,国内外鲜有报 道,是一种有效的途径和方法,值得临床推广与使用。
参考文献略。
原始出处:
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#腹膜外#
36
#黏液瘤#
49
#血管黏液瘤#
28
#侵袭性#
0
#会阴#
43
#腹膜#
32