Clin Gastroenterol Hepatol:多学科讨论:他汀可使慢性肝病患者获益
2017-11-01 常路 环球医学
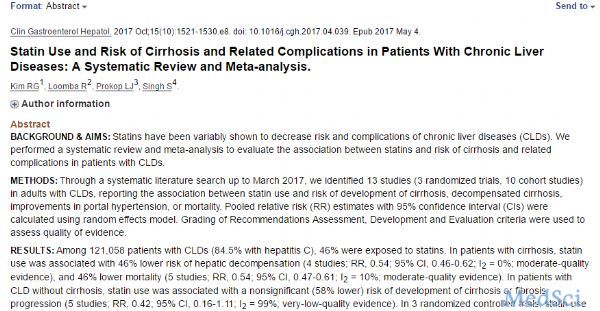
慢性肝病(CLDs)是全世界发病率和死亡率的重要原因。目前,没有预防或逆转肝功能失代偿的药物。他汀类药物是一类正在研究的以确定其对CLDs进展和失代偿影响的药物。2017年10月,发表在《Clin Gastroenterol Hepatol》的一项系统评价和Meta分析评估了他汀和CLDs患者肝硬化及相关并发症风险之间的相关性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#AST#
38
#肝病患者#
40
#GAS#
40
#Gastroenterol#
33
#EPA#
33
#多学科#
35