Cell Metab:FXR对炎性小体的调控与胆汁淤积性脓毒症有何关系?
2017-04-20 MedSci MedSci原创
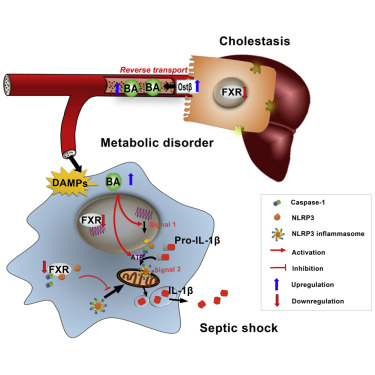
法尼基衍生物X受体(FXR)是一种胆汁酸受体,属核受体超家族成员,在胆汁酸及胆固醇代谢中具重要作用。NLRP3炎性小体作为炎症反应的核心,NLRP3炎症小体可能为各种炎症性疾病的治疗提供新的靶点 。
胆汁淤积是脓毒症的一种常见并发症,且血浆中的胆汁酸可以预测脓毒症相关的死亡率。然而,胆汁淤积加重脓毒症发展的作用机制尚不明确。
在这一期的Cell Metabolism杂志中,来自中国药科大学的郝海平及其同事发现:作为危险相关模式分子(DAMPs)的胆汁酸可以激活炎症状态下巨噬细胞中NLRP3炎性小体的信号1和信号2。在机制方面,胆汁酸可以协同ATP引发长时的钙流和NLRP3炎性小体的激活。在胆汁淤积敏感性实验中,消胆胺(一种胆汁酸螯合剂)可以保护小鼠免于脂多糖诱发的脓毒症,FXR敲除小鼠更易发生内毒素血症休克,而FXR过表达小鼠则反之。
该研究主要明确了:胆汁酸可以激活NLRP3炎性小体的信号1和信号2;胆汁酸通过促进钙流激活了NLRP3炎性小体;FXR是NLRP3炎性小体的负性调控因子;FXR和胆汁酸可以调控脂多糖引起的脓毒症。
该研究提示:胆汁酸和FXR通过控制NLRP3炎性小体在脓毒症中发挥关键作用。因此,靶向FXR可能为胆汁淤积性脓毒症提供一个新的治疗策略。
原始出处:
Hao H, Cao L, Jiang C, et al.Farnesoid
X Receptor Regulation of the NLRP3 Inflammasome Underlies
Cholestasis-Associated Sepsis . Cell Metab. 2017 Apr 4;25(4):856-867.e5. doi: 10.1016/j.cmet.2017.03.007.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#CEL#
39
#MET#
38
#胆汁淤积#
40
#Cell#
38
#Meta#
44
#炎性小体#
48
学习了,谢谢分享
99
学习了,谢谢分享
93
#胆汁#
36
#FXR#
44