Haematologica:ALK阳性间变性大细胞淋巴瘤的特征是重排ALK基因拷贝数增加
2017-07-13 xiaoxiao MedSci原创
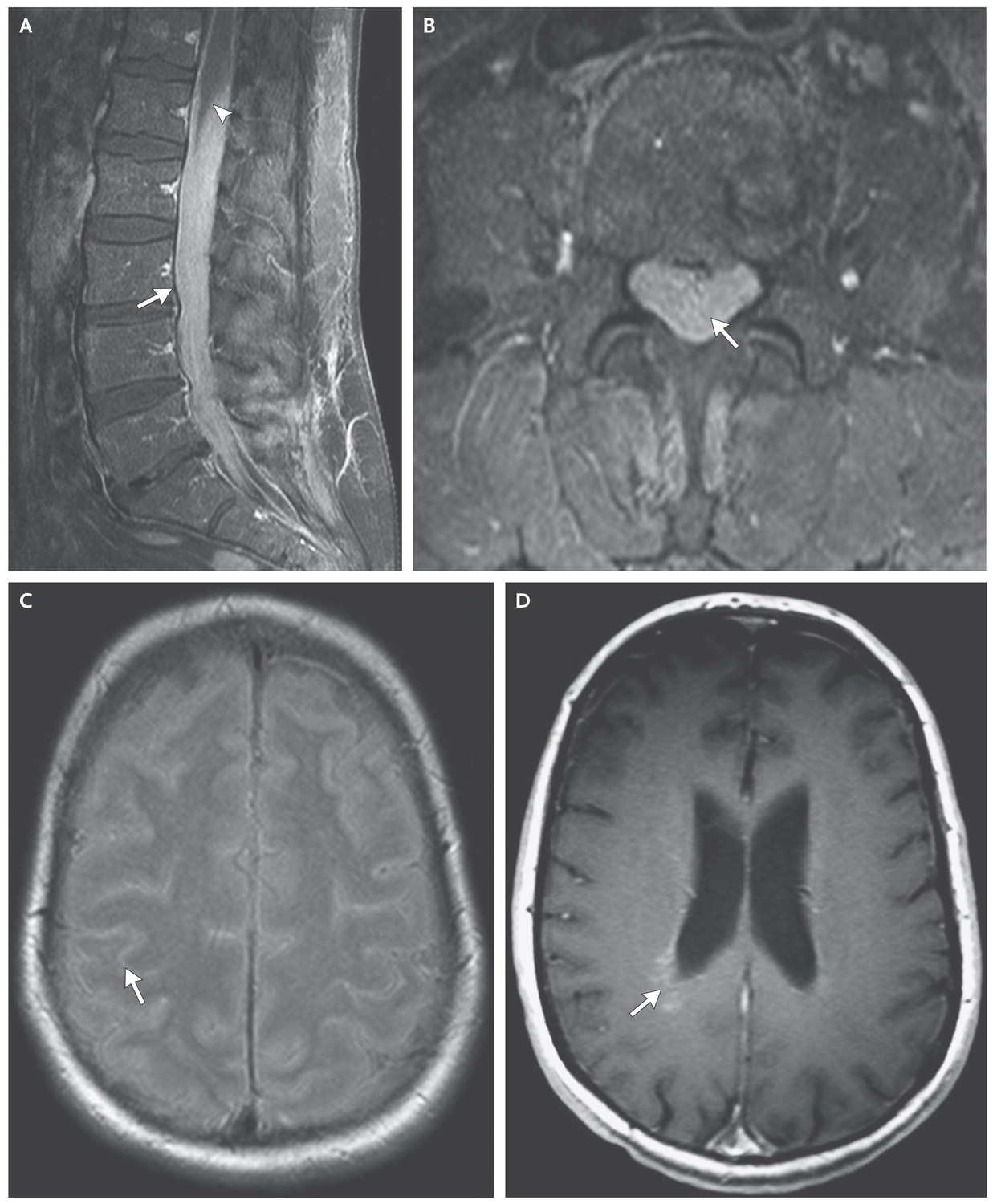
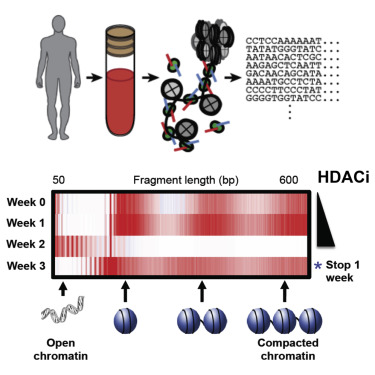
间变性大细胞淋巴瘤(anaplastic large cell lymphoma , ALCL) 亦称 ki-1 淋巴瘤,细胞形态待殊,类似 R-S 细胞,有时可与霍奇金淋巴瘤和恶性组织细胞病混淆。细胞呈 CD30 + ,亦即 Ki-1(+), 常有t(2;5)染色体异常,临床常有皮肤侵犯,伴或不伴淋巴结及其他结外部位病变。免疫表型可为 T 细胞型。 约半数的间变性大细胞淋巴瘤(ALCL
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞淋巴瘤#
31
#ALK阳性#
41
#阳性间变性大细胞淋巴瘤#
41
#拷贝数#
31
#HAE#
37
#EMA#
32
#变性#
39
签到学习了很多人
66