JACC:如何减少他汀类使用中出现的肌肉毒性等副作用?
2017-08-29 sunshine2015 来宝网
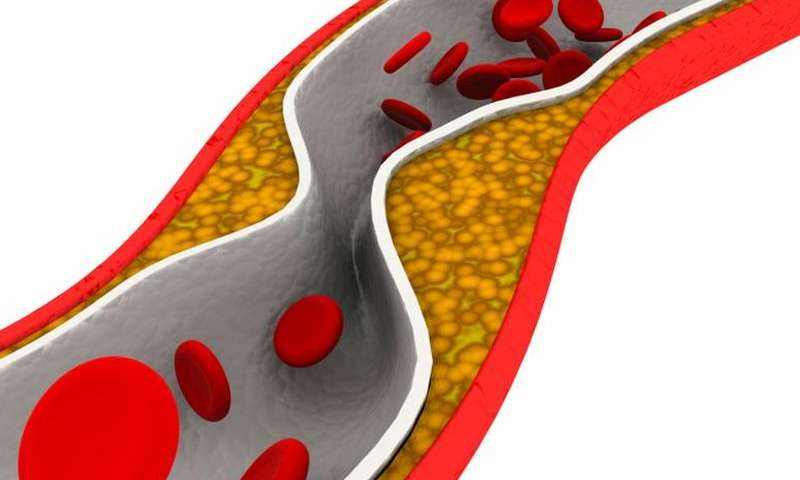
他汀类药物通过降低低密度脂蛋白或“不良”胆固醇来预防心脏病发作非常有效。然而,10%至20%的服用他汀类药物的患者报告肌肉相关症状,包括疼痛和痉挛,限制了他们使用推荐剂量。服用他汀类药物的患者心血管事件的风险很高,导致医疗保健成本上升。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
43
#副作用#
38
学习了学习了学习了学习了学习了学习了学习了学习了
86
#ACC#
0
好好看一下
83
学习了解了解
79