BJC:食管鳞癌患者的多学科治疗策略研究
2016-11-13 MedSci MedSci原创
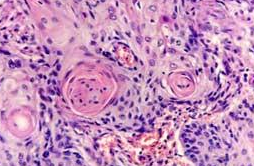
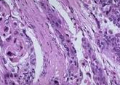
食管局部晚期鳞状细胞癌(SCC)的标准治疗是顺铂结合5-氟尿嘧啶(CF-RT)的放化疗。这个多中心II期临床试验的对象为最初不能手术切除的局部晚期食管SCC患者,评估多烯紫杉醇+顺铂、5 -氟尿嘧啶(DCF)诱导化疗(ICT)和随后转换手术(CS)的安全性与有效性。 研究纳入临床T4和/或不可切除的锁骨上淋巴结转移患者。开始治疗为三个周期的DCF-ICT,此后如果肿瘤可以切除,则进行CS;如
食管局部晚期鳞状细胞癌(SCC)的标准治疗是顺铂结合5-氟尿嘧啶(CF-RT)的放化疗。这个多中心II期临床试验的对象为最初不能手术切除的局部晚期食管SCC患者,评估多烯紫杉醇+顺铂、5 -氟尿嘧啶(DCF)诱导化疗(ICT)和随后转换手术(CS)的安全性与有效性。
研究纳入临床T4和/或不可切除的锁骨上淋巴结转移患者。开始治疗为三个周期的DCF-ICT,此后如果肿瘤可以切除,则进行CS;如果不能切除,则进行CF-RT,剂量为30–40 Gy,此后再次评估能否切除,如果能,则进行CS,如果不能,则完成60 Gy的CF-RT治疗。主要终点为1年总生存率(OS)。
共有48名患者参加研究,41.7%(n = 20)的患者进行了CS,包括DCF-CS (n=18)、DCF-CF-RT40Gy-CS (n=1)和DCF-CF-RT60Gy-CS (n=1)。19例(39.6%)为R0切除者。术后并发症等级大于或等于3的事件包括喉返神经麻痹、肺部感染、伤口感染、肺瘘、吞咽困难(各一例);没有发现CS患者出现严重术后并发症。4例(8.3%)患者CF-RT后出现临床完全缓解。估计1年OS为67.9%,80%置信区间的下限为59.7%。接受DCF-CF-RT60Gy治疗的患者中,发生了1例与治疗相关的死亡。
食管局部晚期鳞状细胞癌患者,对于DCF-ICT后CS这种多学科综合治疗策略,有良好的耐受性和疗效。
原始出处:
Tomoya Yokota1, Ken Kato2, Yasuo Hamamoto3, Yasuhiro Tsubosa.Phase II study of chemoselection with docetaxel plus cisplatin and 5-fluorouracil induction chemotherapy and subsequent conversion surgery for locally advanced unresectable oesophageal cancer.British Journal of Cancer advance online publication 3 November 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#鳞癌患者#
47
很好,不错,以后会多学习
63
#食管#
35
#多学科#
43
#鳞癌#
26