Nature:华人学者首度发现“免疫指挥官”也会疲惫
2017-08-24 佚名 学术经纬
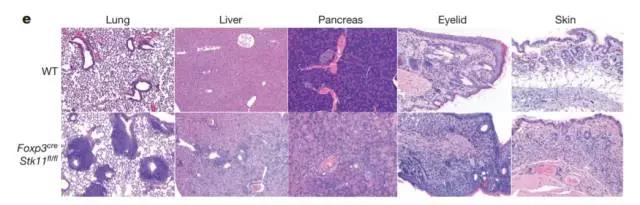
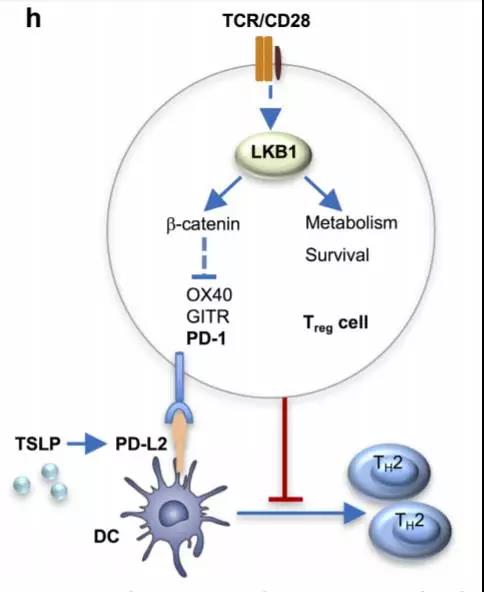
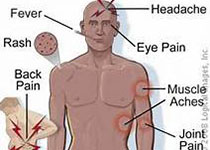
在人体内,有一群叫做调节性T细胞的免疫卫士。它们虽然数量不多,却在免疫系统中扮演了重要的角色——免疫系统之所以不会“暴走”,都是这群细胞的功劳。如果这群细胞出了啥差错,就会诱发哮喘、过敏、甚至是严重的自身免疫疾病。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
29
#华人#
30
#华人学者#
43
学习了.思路可取.
90
学习了谢谢分享
80