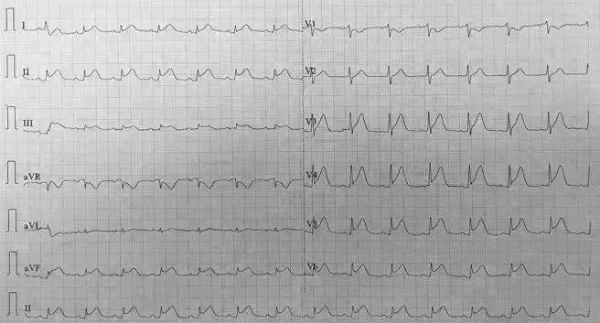
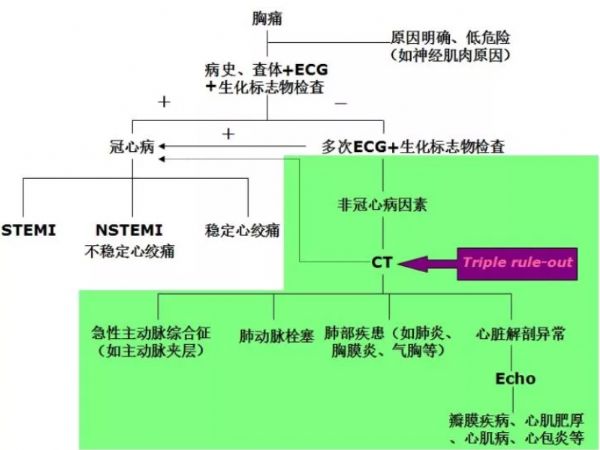
J Emerg Med: 见多了心梗,这一次广泛导联ST段抬高,诊断竟然是……
2018-03-21 YangYang, DieHu, Daoquan Peng 急诊医学资讯
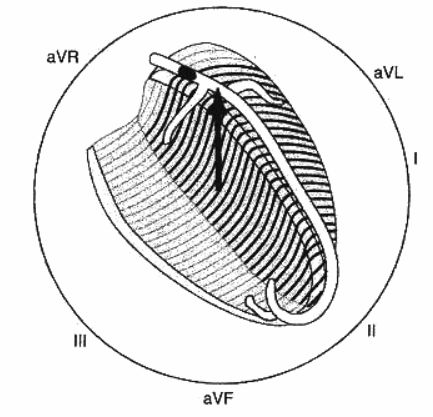
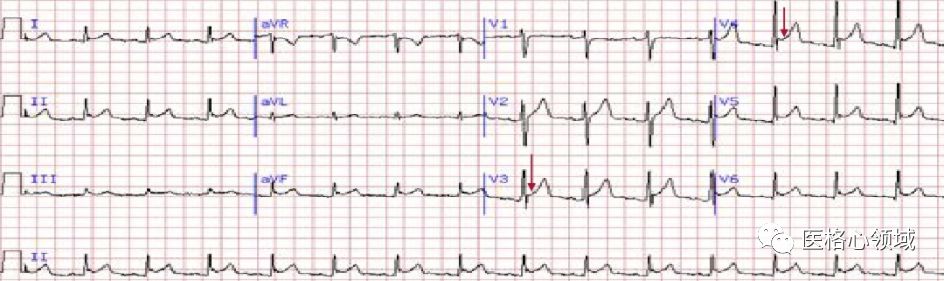
ST段抬高不一定就是心梗。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








好
59
谢谢分享.学习了
65
好
70
#ST段抬高#
20
#Med#
28
#ST段#
26
谢谢分享.学习了
58
学习了
69
不错的文章值得推荐
29