关注|CSCO肾癌诊治指南新版发布,五大亮点等你来看!
2018-05-13 郭军 盛锡楠 李思明 医师报
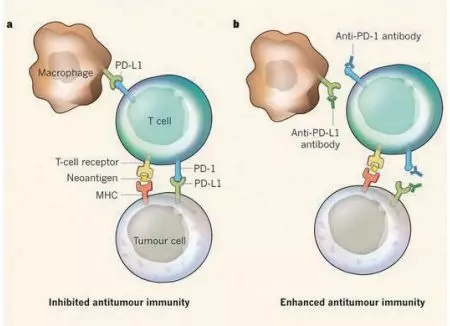
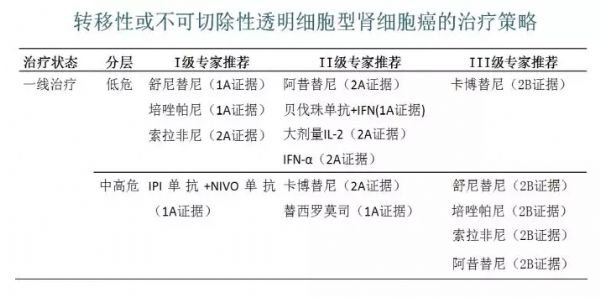
CSCO中国肾癌诊治指南2018版推荐: ☆ 卡博替尼用于中高危晚期肾癌的一线治疗 ☆ 免疫联合治疗作为肾癌晚期一线治疗方式 ☆ 靶向药物与免疫治疗的联合作为晚期肾癌的二线治疗 ☆ 疾病分层将成为晚期肾癌的治疗策略
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了谢谢分享!!
92
#诊治指南#
40
学习了.谢谢分享
81
非常有用
65
学习
71
不错的文章值得拥有
72
学习了.谢谢分享.
21
^_^^_^^_^
31