点赞!华人学者同日再发5篇Nature
2018-04-11 ailsa 生物探索
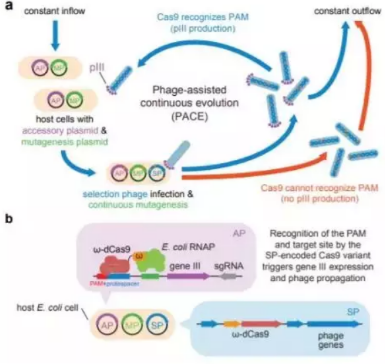
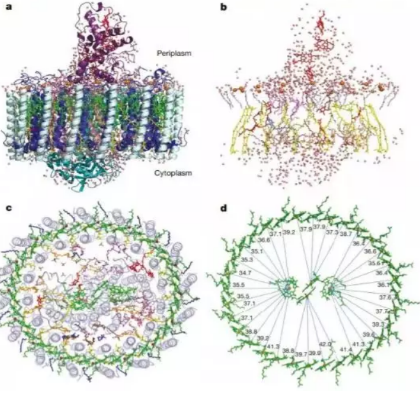
近日,最新一期《自然》上刊登了两项来自华人学者的研究。同时,《自然》也在线刊登了另外3篇华人学者课题组的论文。在这篇报道中,我们将为各位读者介绍这五项最新发现。1刘如谦(David Liu)教授课题组Evolved Cas9 variants with broad PAM compatibility and high DNA specificity图片来源:By ServiceAT (Own







本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
35
确实厉害
65
#华人#
37
#华人学者#
0
学习了
60
学习了.谢谢
65
关注了
53