带血管蒂游离股前外侧肌皮瓣移植治疗巨大头皮缺损1例
2020-02-02 钱海 张伟 雷霆 中国微侵袭神经外科杂志
男,47岁;因颅脑肿瘤术后8年,头皮破溃18个月入院。病人8年前于外院行右额颞胶质瘤切除术,术中予以人工硬脑膜修补、骨瓣复位、钛片固定。术后病理确诊少突胶质细胞瘤,部分间变。18个月前病人切口周围皮肤出现破溃、流脓,自行于当地换药处理。现病人头痛明显加重,头皮破溃面积增大。
1.病历摘要
男,47岁;因颅脑肿瘤术后8年,头皮破溃18个月入院。病人8年前于外院行右额颞胶质瘤切除术,术中予以人工硬脑膜修补、骨瓣复位、钛片固定。术后病理确诊少突胶质细胞瘤,部分间变。18个月前病人切口周围皮肤出现破溃、流脓,自行于当地换药处理。现病人头痛明显加重,头皮破溃面积增大。
查体:右额顶部头皮9处破溃,以原切口边缘为著,最大头皮溃口直径3 cm,溃口下方可见钛钉和钛板外露,伴有黄绿色恶臭脓性分泌物,部分颅骨外露,呈黑褐色。左侧肢体肌力4级,余神经系统查体阴性。
入院时头部MRI提示:右额顶大片指状不均匀长T1、长T2信号影,部分可强化,考虑复发胶质瘤可能。头部CT提示死骨形成。头皮破溃口予以每日换药,根据细菌培养结果予敏感抗生素治疗,拟一期处理头皮感染后,再二期切除复发胶质瘤。病人入院后5d因脑疝急诊行右额顶复发胶质瘤切除术+去骨瓣减压术+头皮及脑内脓肿清除术。
手术方式:沿原手术切口打开皮瓣,见皮下积脓,清创后去除钛片、钛钉,取下原骨瓣,清除硬脑膜外脓液后再扩大骨窗,切开硬脑膜,可见脑表面黄色积脓,予清除。切开脑组织后见深部脓肿腔大小约5 cm×4 cm×3 cm,脓肿壁呈黄色、质韧,吸除脓液后彻底切除脓肿壁,术中右侧脑室额角开放。术毕标本送病理检查。取左股部阔筋膜修补硬脑膜缺损。术中头皮缺损严重,无法严密缝合,先一期转移肌皮瓣,尽可能封闭切口,拟二期行植皮手术。术后继续抗感染治疗及伤口换药。术后病理回报脑脓肿合并间变性少突胶质细胞瘤(WHOⅢ级)。
术后13d,整形外科会诊后行带血管蒂游离股前外侧肌皮瓣移植术。显微镜下彻底游离血管蒂部位的穿支动静脉残端及颞浅动静脉,分别行颞浅动静脉与穿支动静脉端端吻合,术毕血流通畅,间断缝合游离肌皮瓣和头皮皮缘,观察移植肌皮瓣皮色和皮温正常。术后病人恢复良好,无神经系统阳性体征,移植肌皮瓣存活,伤口愈合良好,拆线出院。随访6个月,一般情况良好。
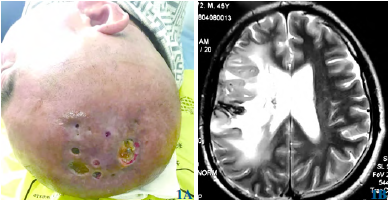
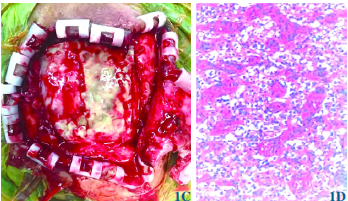
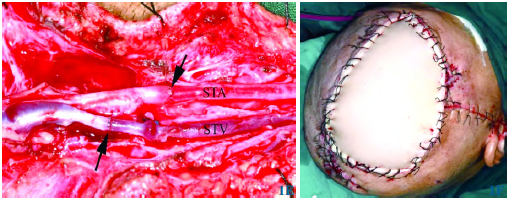
图1 带血管蒂游离股前外侧肌皮瓣修复巨大头皮缺损。1A多处头皮腐烂破溃,可见原手术的内植物;1B头部MRI可见右额顶大片指状不均匀长T1长T2信号影,部分可强化;1C入院5d后因脑疝急诊去除骨瓣,术中可见硬脑膜外遍布脓液,术中头皮缺损严重;1D病理结果示:间变性少突胶质细胞瘤,伴微血管增生、片状坏死及灶状钙化。局部区域呈脑脓肿病理改变(苏木精-伊红染色×200);1E头部伤口清创扩创后,切取右股外侧带血管蒂游离肌皮瓣。左侧为游离肌皮瓣,右侧为颞浅动脉近端颧弓部位。颞浅动脉(STA)、颞浅静脉(STV)分别与穿支动、静脉端端吻合;1F带血管蒂肌皮瓣缝合完毕,皮温、皮色良好
2.讨论
本例系复发胶质瘤合并脑脓肿及头皮感染的复杂病例,入院后颅内病变病情进展迅速,急诊行右额顶复发胶质瘤切除术加去骨瓣减压术以及脓肿清除术。术中发现脑表面覆盖脓苔,颅内脓肿形成,术中去除人工植入物、感染脑膜及死骨,取大腿阔筋膜修补硬脑膜缺损。因病情紧急,一期手术无法完全修复头皮缺损,故二期请整形外科会诊后,选择带血管蒂股前外侧肌皮瓣修补头皮缺损,取得良好疗效。结合本病例并复习相关文献,讨论如下。
头皮缺损的修复一般有一期闭合、负压封闭引流技术(VSD)植皮、皮肤扩张、局部及区域肌皮瓣、游离肌皮瓣等方法。根据缺损部位和面积不同,可以采取不同的方法。如果缺损范围太大或者过于复杂,应采用可靠的软组织如游离肌皮瓣移植闭合缺损。作者考虑本例病人体位及切口护理的需要,决定采用带血管蒂和阔筋膜的股前外侧肌皮瓣修复头皮缺损。在复杂或大面积头皮缺损的治疗中,进行微血管重建的游离组织或肌皮瓣移植已经成为治疗复杂头皮缺损的主要手段,血管吻合的成功与否至关重要。在选择吻合类型时需要考虑受体及供体血管的长度和口径、血管蒂的方向和形状、以及吻合后的张力。PIAZZA等一般首选端端吻合(ETE),仅在颈内静脉上采用端侧吻合术(ETS)。
为防止术后并发症,本例病人术后密切观察肌皮瓣血运,充分补足液体量,并予以红外线皮瓣照射及阿司匹林口服,这些措施有助于肌皮瓣血栓并发症的预防。本例由于合并脑胶质瘤复发及颅内感染,处理尤为棘手,难度和风险均远高于一般的大面积头皮缺损的修复。在修复缺损的同时,需要兼顾到颅内复发肿瘤的处理和颅内感染的控制,一旦颅内感染扩散或者肿瘤切除不彻底均可能带来灾难性的后果。因此本例病人原计划待头皮感染及颅内感染控制后,再二期彻底处理肿瘤复发。但由于病情突然加重,发生脑疝,不得不急诊行手术治疗。
清创时由外向内分步清除脓液并冲洗术野,避免将外部感染源带入颅内,颅内操作时注重周围脑组织的术野保护,彻底清除脓液、脓肿壁以及复发的肿瘤组织,然后取自体阔筋膜严密修补硬脑膜缺损,减少由于肌皮瓣暴露导致感染蔓延至颅内的危险。术后予伤口换药及敏感抗生素治疗,同时予腰大池持续引流,待稳定后行二期肌皮瓣移植。
综上,游离股前外侧肌皮瓣具有面积厚度可变、柔韧性高、血管蒂长度可调的优点,是首选的供体肌皮瓣选择。术中可以根据受区需要定制切取的大小,包括深层和浅层组织、阔筋膜和神经组织等,使用显微血管吻合技术的游离股外侧肌皮瓣更适合于复杂的大面积缺损病例,如合并颅骨缺损、颅内感染甚至是脑脊液漏的严重病人。
原始出处:
钱海,张伟,雷霆,刘方军,刘元波,张勇.带血管蒂游离股前外侧肌皮瓣移植治疗巨大头皮缺损1例[J].中国微侵袭神经外科杂志,2019(01):40-41.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肌皮瓣#
40
#皮瓣移植#
32
#血管蒂#
32
#皮瓣#
31