儿童颈椎管内可疑椎体骨软骨瘤1例
2019-04-25 张鹏 卢斌 刘扬 中国骨与关节损伤杂志
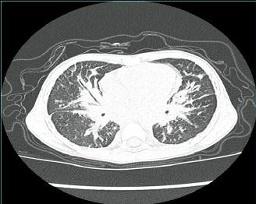
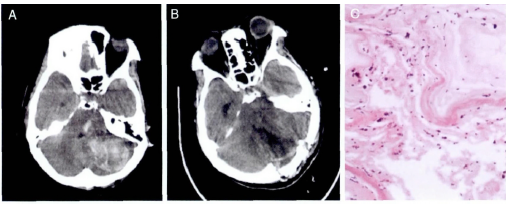
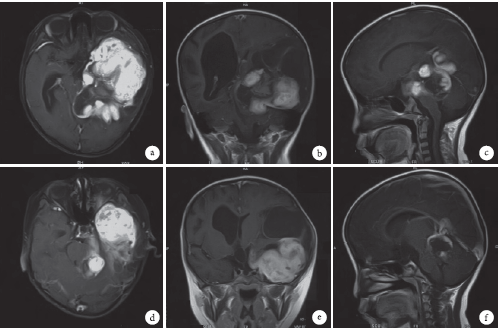
患者,男,8岁,因“外伤致颈背部疼痛、活动受限1周”入院。门诊查颈椎CT显示寰枢关节半脱位,C3、4椎管内可见片状致密影。门诊以“寰枢关节半脱位”收治,专科查体:颈部疼痛,向左侧偏斜,颈部活动受限;四肢运动、感觉未见明显异常;生理反射存在,病理征未引出。临床诊断:寰枢关节半脱位,颈椎管占位。入院第2天颈椎MRI显示椎管内占位与椎体后缘相连,范围0.7CM×1.2CM,局部后纵韧带掀起致局部椎管狭窄
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#椎管#
38
#骨软骨#
35
#椎管内#
46
学习了
80
#椎体#
32
#软骨瘤#
31