JAHA:非阻塞性冠状动脉心肌梗死患者预后和死亡率预测因素
2019-07-09 xing.T MedSci原创
由此可见,MINOCA患者和阻塞性冠状动脉疾病心肌梗死患者临床结局相似。肾素-血管紧张素系统阻滞剂和他汀类药物的使用与MINOCA患者的死亡率降低相关。
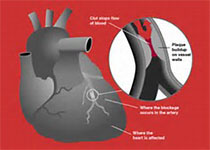
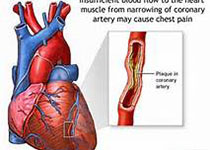
非阻塞性冠状动脉(MINOCA)心肌梗塞是一种异质性疾病,其预后和死亡率预测仍不明确。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在比较MINOCA与梗死性冠状动脉疾病心肌梗死之间的预后,并使用全国性、多中心和前瞻性登记中心来确定MINOCA与全因死亡相关的因素。
在入组的13104名连续就诊患者中,选择了未接受过冠状动脉造影的有明显冠状动脉疾病史的患者。主要结果是2年全因死亡。次要结果是心脏死亡、非心脏死亡、再梗塞和重复血运重建。
MINOCA患者(n=396)和梗阻性冠状动脉疾病心肌梗死患者(n=10 871)全因死亡率相似(9.1% vs. 8.8%;风险比[HR]为1.04; 95%CI为0.74 -1.45; P=0.83)。心脏死亡、非心脏死亡和再梗塞的风险在两组之间无显著差异(HR为0.82; 95%CI为0.53-1.28; P=0.38; HR为1.55; 95%CI为0.93-2.56; P=0.09 ; HR为1.23; 95%CI为0.65-2.31; P=0.38)。MINOCA患者重复血运重建发生率较低(1.3% vs. 7.2%; HR为0.17; 95%CI为0.07-0.41; P<0.001)。在多变量回归和倾向得分匹配后,结果是一致的。在一个多变量模型中,研究人员发现了MINOCA患者全因死亡的几个重要预测因子,包括不使用肾素-血管紧张素系统阻滞剂(HR为2.63; 95%CI为1.08-6.25; P=0.033)和他汀类药物(HR为2.17; 95%CI为1.04-4.54; P=0.039)。
原始出处:
Eun Ho Choo.et al.Prognosis and Predictors of Mortality in Patients Suffering Myocardial Infarction With Non‐Obstructive Coronary Arteries.JAHA.2019.https://www.ahajournals.org/doi/full/10.1161/JAHA.119.011990
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#阻塞#
27
#患者预后#
24
#预测因素#
29
#AHA#
20
学习
59