Cell Stem Cell:抑制骨内膜血管重塑有望重启AML患者的正常造血!
2018-01-09 MedSci MedSci原创
造血干细胞寄居于骨髓中,它们从包括多种细胞包括内皮细胞和多种血管前体间充质细胞中接受存活和分化的信号。
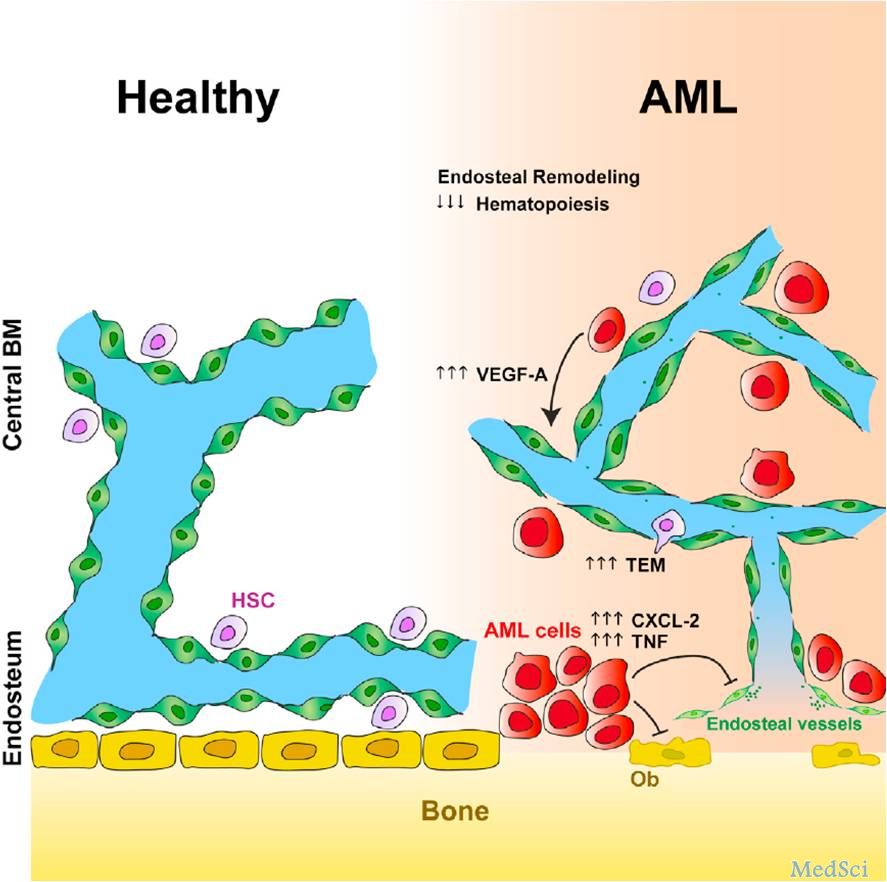
造血干细胞寄居于骨髓中,它们从多种细胞包括内皮细胞和多种血管前体间充质细胞中接受存活和分化的信号。肿瘤细胞的持续生长和对化疗药物耐受被认为是由高度血管化的骨髓恶性环境造成的。急性髓系白血病是一种侵袭性的白血病伴随着致命的血细胞减少。AML在60岁以上的老年患者的治愈率约为5%-15%。
在白血病发病过程中骨髓微环境被重塑,进而支持其病理发展过程。急性髓系白血病细胞能产生血管生长因子从而推进骨髓微环境的进一步重塑。但是相应的抗血管治疗不能提高病人的治疗效果。通过活体显微镜,科学家们发现AML疾病发生过程中会出现骨髓中央和骨内膜血管的差异性重塑。骨内AML细胞产生前炎症因子以及抗血管生成因子,并且逐渐降解骨内膜内皮细胞,基质细胞和成骨细胞,而中央骨髓持续血管化,并且脾脏血管微环境不断扩增。重塑骨内区域能降低对非白血病造血干细胞支持能力,从而导致正常造血缺陷。用小分子地塞米松或者基因方法保护骨内膜内皮细胞能挽救HSCs丢失,提高化疗效果,提高患者生存率。这些结果表明防止骨内膜血管的降解能促进目前治疗AML的范式。
原文出处:Duarte D, Hawkins E D, Akinduro O, et al. Inhibition of endosteal vascular niche remodeling rescues hematopoietic stem cell loss in AML[J]. Cell stem cell, 2017.DOI: 10.1016/j.stem.2017.11.006
本文由梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#内膜#
30
#CEL#
24
#血管重塑#
45
#stem cell#
32
#Cell#
33
#STEM#
34
#造血#
26