NATURE:新抗原疫苗在Ib期胶质母细胞瘤试验中产生肿瘤内T细胞应答
2018-12-22 海北 MedSci原创
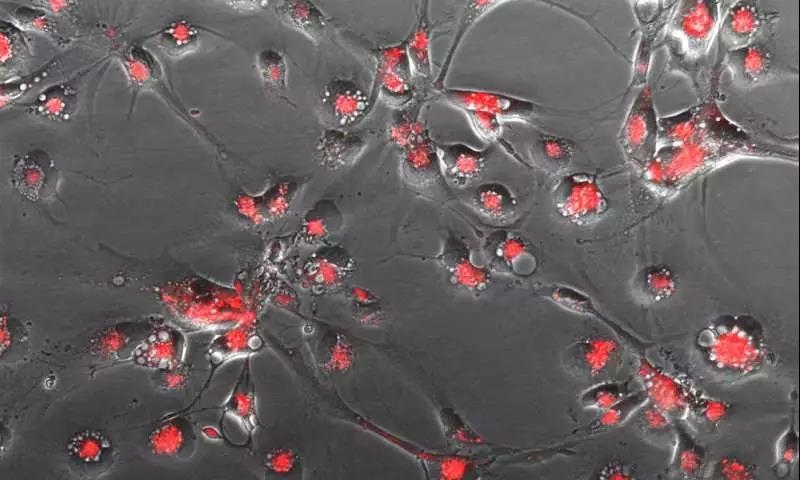
源自肿瘤特异性蛋白质编码突变的新抗原可以免于中枢耐受,并且其可产生强烈的免疫应答,作为促进肿瘤排斥的真正抗原。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Ib期#
32
#Nat#
37
#T细胞应答#
44
#母细胞瘤#
38
#新抗原疫苗#
31
#胶质母细胞#
29
#细胞瘤#
26
#抗原#
24