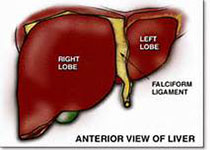
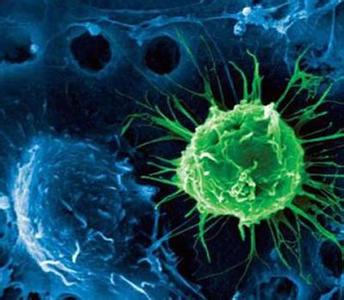
Gastroenterology:超声波+血检 肝癌早期检测提高不只一点点
2018-02-12 石岩 环球医学
在大多数癌症发病率呈下降趋势的今天,肝癌却异军突起,不减反增。在美国,肝癌是发病率上升最快的固体肿瘤,在过去10年间,每年增加2.7%。肝癌如果能被早期发现,医生就可以进行治愈性治疗,从而让患者活得更久。然而,“理想很丰满,现实很骨感”,事实是大多数肝癌患者被发现时已是后期,当然也不可能进行治愈性治疗,因此他们的生存率很低。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Gastroenterol#
35
#AST#
37
#GAS#
42
#超声波#
36
学习一下谢谢
58
#血检#
28
#Gastroenterology#
37
学习一下谢谢
62