BMJ:质子泵抑制剂(PPIs)可降低患者心肌梗死后消化道出血的风险
2015-10-20 崔倩 译 MedSci原创
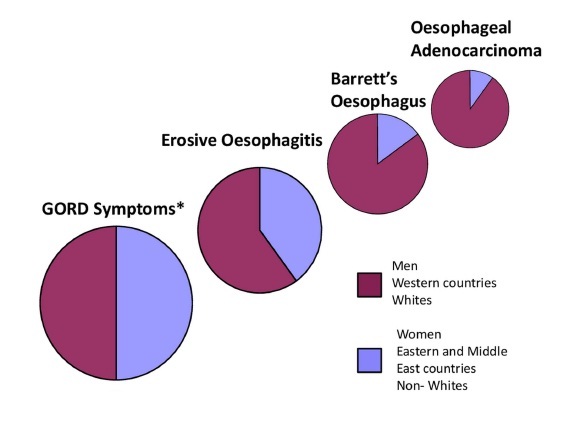
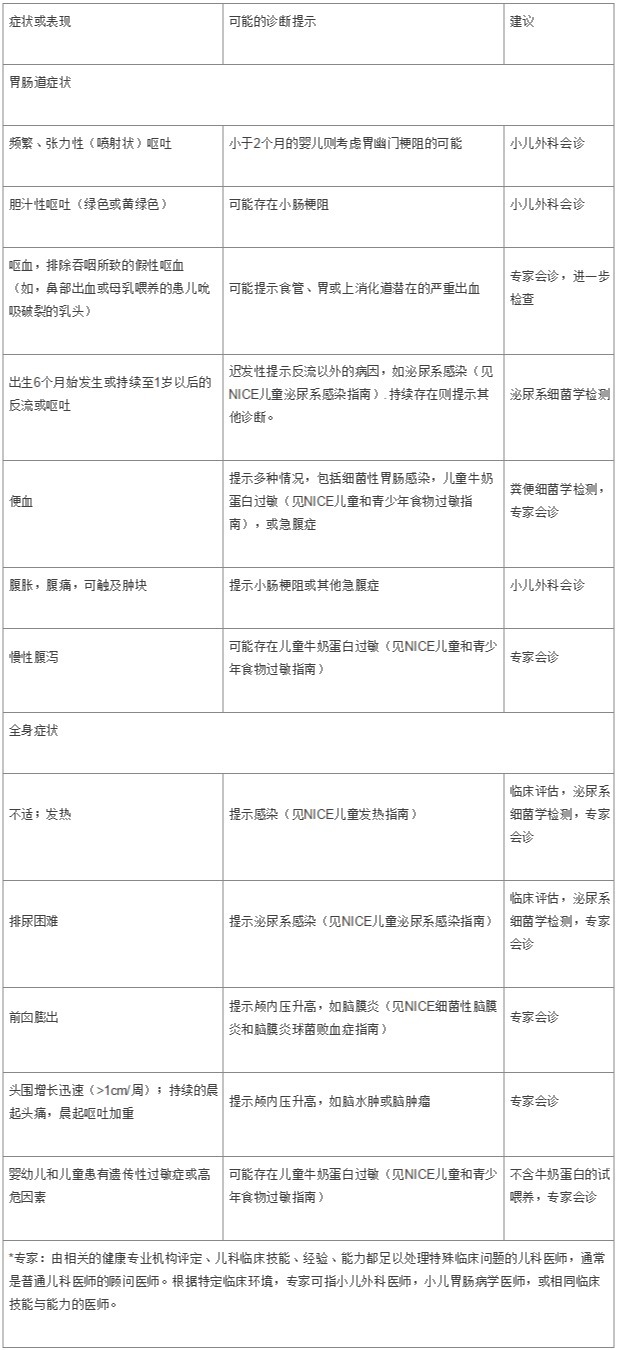
质子泵抑制剂(PPIs)对心肌梗死后患者服用抗血栓形成剂并使用的非甾体类抗炎药(NSAIDs)治疗后消化道出血的风险的影响是怎样的呢?这是一个全国性的队列研究,是以1997年和2011年之间链接丹麦所有医院的行政登记资料为基础的。这些研究参与者均为30岁及以上,并被确诊为第一次发生心肌梗死,且出院后存活至少30天。研究人员使用调整时间相关的Cox回归模型评估了根据NSAIDs加抗血栓治疗,PPIs
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#质子泵#
37
#BMJ#
33
#抑制剂#
32
赞
133
不错的选择
92
临床早就常规应用
76
#PPIs#
43
#消化道#
23
?
101