Neurology:颈椎动脉支架置入术后再狭窄的光学相干断层扫描诊断与治疗评价
2019-01-31 zyx整理 神经科病例撷英拾粹
65岁男性,由于支架内再狭窄(in-stent restenosis,ISR)接受了球囊血管成形术和再次颈动脉支架置入术(carotid artery stenting,CAS)。
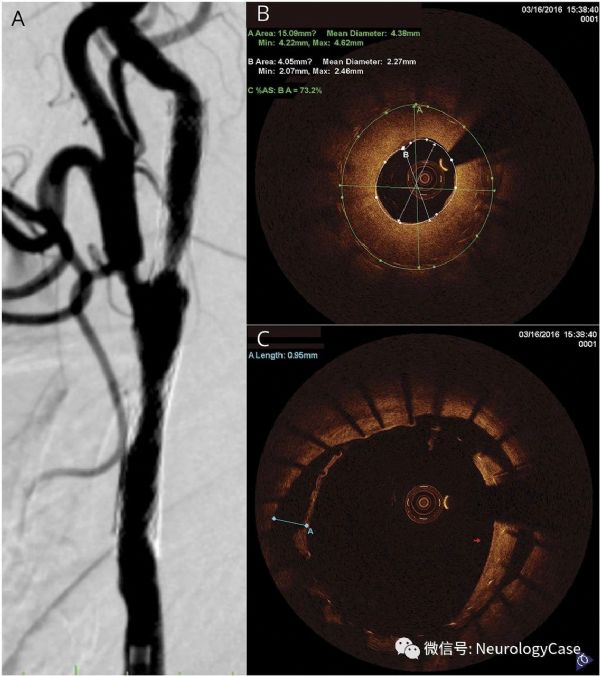
65岁男性,由于支架内再狭窄(in-stent restenosis,ISR)接受了球囊血管成形术和再次颈动脉支架置入术(carotid artery stenting,CAS)。血管内光学相干断层扫描(OCT)可见严重的ISR伴纤维化新生内膜生长(图1)。6.0×30mm球囊血管成形术后,OCT可见内膜破裂和动脉夹层(图2)。在8.0×40mm支架完全扩张后,OCT显示支架支柱放置好,但可见支架支柱间隙组织突出(图2)。OCT可用于CAS后内膜增生的测量并观察术中内膜破坏和支架支柱放置情况。
(图1:A:血管造影可见ISR;B:严重ISR[73.2%],支架中部展开的支架支柱上可见纤维化新生内膜生长;C:颈动脉分叉层面可观察到支架贴壁不良,支架支柱新生内膜形成和未愈合的动脉夹层)
(图2:A:颈内动脉狭窄段可见大量内膜破裂;B:球囊血管成形术所致的动脉夹层;C:颈内动脉的狭窄段可见明显的组织突出;D:破裂内膜附着于规则的管腔轮廓,所剩空间很小)
原始出处:
Liu R, Yin Q, Li M, et al. Diagnosis and treatment evaluation of in-stent restenosis of carotid artery stenting using optical coherence tomography. Neurology. 2019 Jan 8;92(2):99-100.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Neurol#
40
#置入术#
53
#诊断与治疗#
41
#评价#
38
#再狭窄#
58
#光学相干断层扫描#
42