Oncotarget:靶向浸润性肥大细胞改善良性前列腺增生治疗效果
2017-08-19 Emma MedSci原创
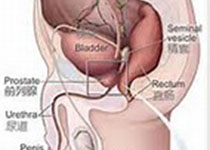
良性前列腺增生(BPH)主要是由于老年人性激素代谢障碍导致的不同程度腺体和(或)纤维,肌肉组织增生而造成前列腺体积增大,正常结构破坏并引起一系列功能障碍的疾病,一般症状体征是尿频,排尿困难,尿潴留。
良性前列腺增生(BPH)主要是由于老年人性激素代谢障碍导致的不同程度腺体和(或)纤维,肌肉组织增生而造成前列腺体积增大,正常结构破坏并引起一系列功能障碍的疾病,一般症状体征是尿频,排尿困难,尿潴留。不及时治疗或治疗不当会引起急性尿潴留,泌尿道感染,膀胱憩室,结石,肾积水,血尿,肾功能衰竭等并发症。有研究提示,肥大细胞可能渗入良性前列腺增生(BPH)组织,因此研究人员调查了肥大细胞在BPH发展中的作用。
研究发现,与正常前列腺相比,人类BPH组织中存在更多的肥大细胞。在体外共培养系统中,BPH-1前列腺细胞促进肥大细胞的活化和迁移, 肥大细胞反过来刺激BPH-1细胞增殖。分子分析表明,肥大细胞来源的白介素6(IL-6)可以激活BPH-1细胞中的STAT3 /细胞周期蛋白D1信号。阻断IL-6或STAT3部分逆转肥大细胞增强BPH-1细胞增殖的能力。此外,在本研究中发现前列腺组织中的肥大细胞浸润与总IPSS(国际前列腺症状评分,检测下尿路症状严重程度的量表)和IPSS-S呈正相关。
研究结果表明,BPH组织浸润性肥大细胞可通过IL-6/STAT3/细胞周期蛋白D1信号促进BPH发展。因此,靶向浸润性肥大细胞可能会改善BPH的治疗效果。
原始出处:
Ou Z, et al. Infiltrating mast cells enhance benign prostatic hyperplasia through IL-6/STAT3/Cyclin D1 signals. Oncotarget. 2017 Jul 22. doi: 10.18632/oncotarget.19465.
本文系梅斯医学(MedSci)原创翻译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#治疗效果#
32
#target#
42
#良性前列腺增生#
62
#肥大细胞#
34
谢谢分享,学习了
65
学习了受益匪浅
75