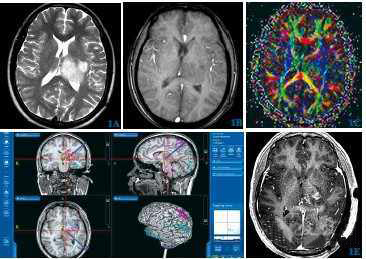
Radiology:高、低级别星形细胞瘤的鉴别
2018-02-27 shaosai MedSci原创
目的:评价由动态磁敏感增强(DSC)MR成像产生的动脉输入函数(AIFs)或AIFDSC值在鉴别低、高级胶质瘤时,能否改善动态对比(DCE)MR成像药物动力学参数(PK)的诊断准确性和可靠性,并与DCE MR成像所获得的AIF进行比较(AIF DCE)。
目的:评价由动态磁敏感增强(DSC)MR成像产生的动脉输入函数(AIFs)或AIFDSC值在鉴别低、高级胶质瘤时,能否改善动态对比(DCE)MR成像药物动力学参数(PK)的诊断准确性和可靠性,并与DCE MR成像所获得的AIF进行比较(AIF DCE)。
材料与方法:本次回顾性研究共纳入226例经病理证实胶质瘤(世界卫生组织分级,Ⅱ级=21,Ⅲ级=53,Ⅳ级=152;异柠檬酸脱氢酶突变体,11.95%(27/226);1p19qco缺失0%[0/226])患者(男138例,女88例;平均年龄52.27岁±15.17岁;范围:24-84岁)。所有病人术前均行DSC及DCE MR检查,获取每一幅图像的AIF DSC 和 AIF DCE。用后处理软件处理两组AIFs的容积转移常数(K trans),血管等离子空间体积(Vp),血管外间隙容积(Ve)。用受试者特性曲线(ROC)分析比较各参数的诊断准确性。采用组内相关系数(ICCs)和Bland-Altman方法进行评估可靠性。
结果:AIFDSC的K trans和v e 值比AIFDCE在鉴别低、高级胶质瘤时更准确(ROC曲线下面积:平均 K trans,0.796vs.0.995; v p,0.848 vs 0.728; v e,0.875 vs 0.581),相关性比较中,这三个参数AIF DSC优于AIFDCE要好(K trans, 0.737 vs 0.095; v p, 0.848 vs 0.728; v e, 0.875 vs 0.581)。在AIF分析中,AIF DSC 在最大信号强度(0.837 vs 0.524),斜率(0.800 vs 0.432)相关性比较中优于 AIF DCE。
结论:DCE MR成像药物动力学参数产生的AIF DSC优于AIF DCE在鉴别低、中胶质瘤时有较好的诊断准确性和可靠性。
原始出处:
You SH, Choi SH, Kim TM. et al.Differentiation of High-Grade from Low-Grade Astrocytoma: Improvement in Diagnostic Accuracy and Reliability of Pharmacokinetic Parameters from DCE MR Imaging by Using Arterial Input Functions Obtained from DSC MR Imaging.Radiology.DOI: 10.1148/radiol.2017170764
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了谢谢分享!!
56
#细胞瘤#
27
了解一下.谢谢分享!
56
学习
71
学习一下谢谢分享
0
不错的文章值得拥有
60
学习了.涨知识了!
22