系统性红斑狼疮患者并发急性泛发性表皮松解综合征与血栓风暴一例
2019-05-10 小参考 医学参考报皮肤病与性病学频道
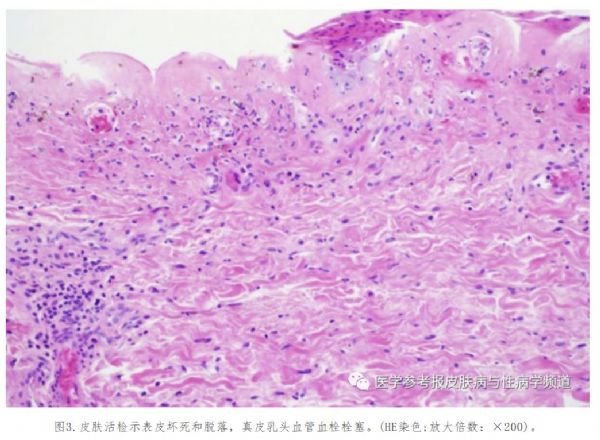
美国德克萨斯州Elise Burger等报道一位全身泛发性水疱性皮炎伴凝血障碍与高凝状态的39岁女性患者,该患者有系统性红斑狼疮病史(抗核抗体,1:1280;抗Sm抗体+;dsDNA+;尿蛋白)和免疫性血小板减少性紫癜病史。该患者最初出现了抗核抗体样综合征,并接受了包括两性霉素B、哌拉西林/他唑巴坦和头孢唑啉在内的多种抗菌药物治疗。随后其面颈部、乳房、手臂上出现尼氏征阳性的褐色斑块。上胸部、腹部、
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#泛发性#
41
#并发#
34
#系统性#
38
#狼疮#
33
#综合征#
32
#红斑#
29