BMC Cardiovasc Disord:新研究支持中国糖尿病患者使用他汀,他汀可使死亡和心血管病风险减半
2017-07-18 许菁 中国循环杂志
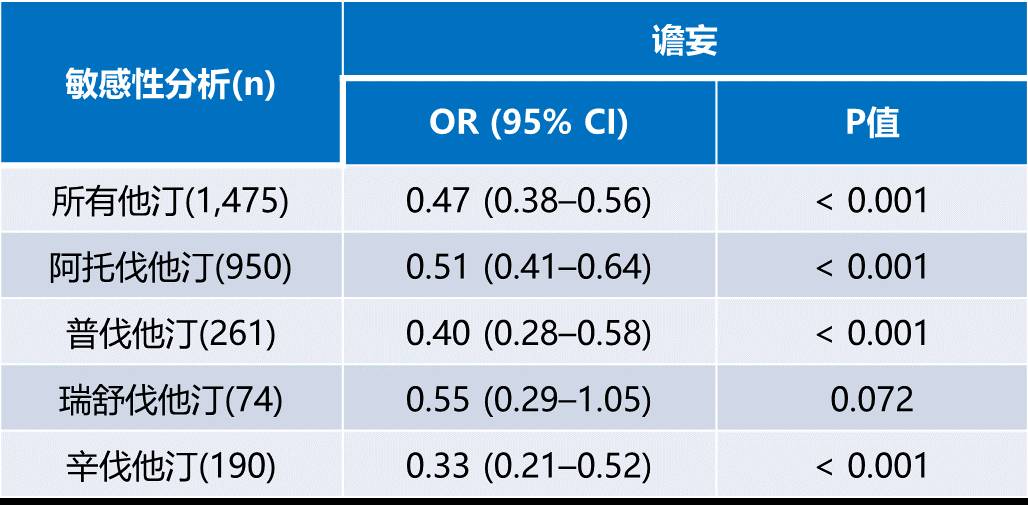
香港大学学者近期报告,对于糖尿病患者的一级预防,支持低密度脂蛋白胆固醇(LDL-C)降得越低,获益越大的观点。 如果使LDL-C降至2.6 mmol/L以下,心血管病风险和全因死亡风险均降低50%以上。 研究者回顾性观察了10 104例糖尿病患者,并与对照组进行了匹配。 研究发现,与未应用他汀者相比,他汀应用者的LDL-C水平降低了1.21 mmol/L。 在中位随访50.5个月后,应用他
香港大学学者近期报告,对于糖尿病患者的一级预防,支持低密度脂蛋白胆固醇(LDL-C)降得越低,获益越大的观点。
如果使LDL-C降至2.6 mmol/L以下,心血管病风险和全因死亡风险均降低50%以上。
研究者回顾性观察了10 104例糖尿病患者,并与对照组进行了匹配。
研究发现,与未应用他汀者相比,他汀应用者的LDL-C水平降低了1.21 mmol/L。
在中位随访50.5个月后,应用他汀患者的心血管病风险降低了54%,死亡风险下降62%。
如果应用他汀使LDL-C达到<2.6 mmol/L, 则心血管病风险降低50.9%,全因死亡风险降低51.3%。
但是,研究者发现,我国合并高脂血症的糖尿病患者的他汀应用严重不足,在这些患者中,未服用他汀的患者数量是服用他汀患者数量的5倍。
研究者认为,患者有可能担忧药物对肝脏有副作用,影响了药物应用。
原始出处:
Fung CSC, Wan EYF, Chan AKC, Lam CLK. Statin use reduces cardiovascular events and all-cause mortality amongst Chinese patients with type 2 diabetes mellitus: a 5-year cohort study. BMC Cardiovasc Disord. 2017,17: 166.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMC#
26
#Disord#
26
#血管病#
32
#ASC#
21
#Dis#
0
#糖尿病患者#
16
继续学习中谢谢
38
学习了谢谢分享
46
学习了,很好的研究
54