病例介绍
主诉 腰痛3年,周身痛1年,加重1个月。
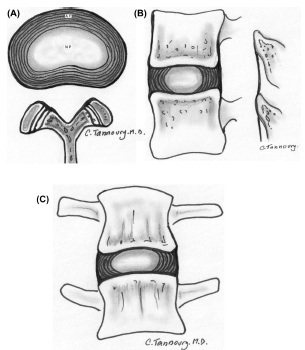
现病史 患者3年前无明显诱因出现腰痛,就诊于当地医院,诊断为腰椎间盘突出症,给予理疗、按摩等治疗,症状略有缓解,呈短暂性,之后症状逐渐加重。1年前开始出现周身痛,以四肢、关节痛为主,伴有周身乏力及食欲减退,无恶心、呕吐、腹痛、夜尿增多、尿痛、血尿等不适。近1个月来疼痛较前明显加重,20余天前就诊于当地医院,查血钙、ALP升高,血磷降低,泌尿系超声示:双肾结石。甲状腺B超示:甲状腺左叶低回声结节(3.9c m×1.9c m),右叶小结节(0.7c m×0.4c m),甲状旁腺素升高,以甲状旁腺功能亢进症收入院,患者自发病以来,精神、饮食、睡眠尚可,大、小便正常。
个人史 无烟、酒等不良嗜好。
既往用药史 入院前曾口服硝苯地平缓释片20mg,1日1次;阿司匹林肠溶片75mg,1日1次。
过敏史 对青霉素类药物过敏。
【体格检查】
一般状况 男性,55岁,身高175c m,体重67kg,发育正常,营养中等。神志清楚,查体合作。
生命体征 T 36﹒4℃,P 94次/分,R 22次/分,BP 133/87mmHg。
皮肤 全身皮肤黏膜无黄染,无皮下出血、皮疹,无肝掌及蜘蛛痣。全身浅表淋巴结未及肿大。
五官 头颅无畸形,球结膜无水肿,巩膜无黄染,双侧瞳孔正大等圆,直径约3mm,对光反射灵敏。耳鼻检查无异常。口唇无发绀,伸舌居中。咽无充血,扁桃体无肿大。
颈部 颈软,气管居中,甲状腺左叶可触及一大小约3c m×2c m肿物,界清,表面光滑,无压痛,随吞咽上下移动,右叶及峡部未及异常,无颈静脉怒张,未触及肿大淋巴结。
胸部 胸廓对称,无畸形,双侧呼吸动度对称,语颤正常,叩诊清音,双肺呼吸音清晰,未闻及干湿啰音。
心脏 心前区无隆起,心率94次/分,心律齐,心音有力,各瓣膜听诊区未闻及杂音。
腹部 腹部平坦,无腹壁静脉曲张。腹软,无压痛、反跳痛及肌紧张,肝脾肋下未及。叩诊鼓音,移动性浊音阴性,双肾区无叩击痛。肠鸣音正常存在。
四肢 脊柱无畸形,腰椎椎体压痛,四肢关节无压痛,肌力、肌张力正常。双下肢无水肿。双足背动脉搏动可。
神经系统 生理反射存在,双巴氏征阴性。脑膜刺激征阴性。
辅助检查
1﹒电解质Na 139﹒7mmol/L,K 4﹒98mmol/L,Ca 3﹒62mmol/L ↑,Phos 0﹒53mmol/L ↓,Mg 0﹒48mmol/L ↓。
2﹒24小时尿 钙6.52mmol/L,磷7.8mmol/L。
3﹒PTH 191﹒0p mol/L ↑。
4﹒心肌酶MYO73.9ng/ml(0~90ng/ml),CK 63﹒0U/L(25~192U/L),CK MB 13﹒0U/L(0~24U/L),LDH 163﹒0U/L(80~240U/L),α‐HBDH 144﹒0U/L(95~250U/L)。
5﹒血常规WBC6.17 ×109/L,RBC 4﹒4 ×1012/L,HGB 135g/L,PLT 274 ×109/L。
6﹒肝功能TBIL 4﹒32μmol/L,IBIL 2﹒60μmol/L,DBIL 1﹒72μmol/L,ALT 25﹒0U/L,AST 12﹒0U/L,ALP 1487U/L ↑(30.0~120.0U/L)。
7﹒肾功能 尿素氮8.29mmol/L,肌酐109.4μmol/L,尿酸418.8μmol/L。
8﹒血脂CHOL 5﹒26mmol/L,T G 3﹒06mmol/L,HDL 0﹒69mmol/L,LDL 3﹒76mmol/L。
9﹒甲状腺功能FT34﹒35p mol/L,FT415﹒8p mol/L,TSH 0﹒68μI U/ml。
10﹒泌尿系超声 ①双肾结石;②膀胱未见明显异常;③双侧输尿管未见明显扩张。
11﹒骨盆正位片 ①左侧骶髂关节显示不清,双侧髋臼内低密度影,建议CT或MRI进一步检查;②骨盆及所见腰椎骨质密度减低,部分骨结构模糊,结合临床符合甲旁亢表现;③腰椎骨质增生。
入院诊断
1﹒原发性甲状旁腺功能亢进症?
2﹒甲状腺囊肿?
3﹒高血压2级,高危。
诊疗经过 住院后高钙血症诊断明确,立即给予以下处理:
Ⅰ级护理
0﹒9%氯化钠注射液4000ml/24h(24小时内持续静脉滴注0.9%氯化钠注射液共计4 000ml)ivgtt
呋塞米注射液40mg入壶qd
鲑鱼降钙素注射液300I U +0.9%氯化钠注射液500ml ivgtt(缓慢注射,6小时以上)qd
伊班磷酸钠注射液4mg +0.9%氯化钠注射液500ml ivgtt(缓慢注射,2小时以上)qd
1﹒治疗高钙血症入院后患者高钙血症诊断明确,血清钙超过2.75mmol/L即为高钙血症,临床上常常根据血清钙水平将高钙血症分为轻、中和重度,血清钙<3mmol/L为轻度,介于3~3.5mmol/L之间为中度,>3.5mmol/L为重度。血清钙>3.5mmol/L时,可伴有一系列严重的临床征象,称为高钙危象。当血钙>3.5mmol/L时,不管有无临床症状,均需立即采取有效措施降低血钙。该患者血清钙升高明显,>3.5mmol/L,所以应立即处理高钙血症。措施包括:①大量补液,根据失水情况每天补充生理盐水4~6L;②给予呋塞米40~60mg静脉注射,促进尿钙排出;③给予降钙素2~8U/(kg·d),肌内注射,降低血钙,改善骨痛的症状。
高血钙的病因很多,其中90%以上的高钙血症是由原发性甲旁亢和恶性肿瘤引起的,因此进行两者的鉴别非常重要,诊断需要综合考虑患者的病史、症状、体征、实验室和影像学等检查结果。本例患者血PT H升高明显,甲状旁腺超声:甲状旁腺区未见占位性病变。甲状旁腺核素扫描:静脉注射Tc‐99m‐MIBI,20分钟、2小时行颈前显像,结果如下:初始相(20分钟)甲状腺显影,轮廓尚规整,内部核素尚均匀,颈前及上胸部未见异常放射性浓聚影。延迟相(2小时)甲状腺左叶上极区仍可见核素浓聚影,甲状腺左叶下极及右叶明显变淡,内部仅有少量核素残留。甲状腺双时相显像示:甲状腺左叶上极区异常核素聚集,考虑为功能亢进的甲状旁腺组织。患者肾脏超声有肾结石,骨盆拍片示骨质疏松,肾功能正常,肿瘤检查(蛋白芯片)阴性,所以诊断为原发性甲状旁腺功能亢进症。患者甲状腺超声示:甲状腺右叶等回声占位性病变,甲状腺左叶低回声占位性病变。甲状腺CT左侧甲状腺后上方椭圆形肿块,伴左侧颈部淋巴结肿大。
2﹒术前准备并手术由于患者周身疼痛明显,难以忍受,经上述治疗5天后患者疼痛减轻,血清钙降至3.0mmol/L,进行了术前常规检查,为手术做准备。患者既往口服阿司匹林肠溶片,为避免术中出血较多,停用。术前准备充分后在全麻下行甲状腺及甲状旁腺肿物切除术,术中冷冻切片示甲状旁腺腺瘤,给予肿物切除及周围淋巴结清扫。术后第3天复查电解质:Ca 2﹒42mmol/L,Phos 0﹒65mmol/L ↓,Mg 0﹒39mmol/L ↓,骨痛较前明显好转。术后病理示:甲状旁腺腺瘤,另送右侧甲状腺病理为结节性甲状腺肿伴腺瘤样增生。切口恢复良好,拆线后出院。
出院诊断
1﹒原发性甲状旁腺功能亢进症:甲状旁腺腺瘤,高钙危象。
2﹒结节性甲状腺肿。
3﹒高血压2级,高危。
病例特点与诊断要点
1﹒病史 3年的腰痛病史,曾经诊断为腰椎间盘突出症,给予理疗、按摩等治疗,病情无明显好转,并有加重趋势。1年前开始疼痛范围逐渐扩大至全身,以四肢、关节痛为主,并出现了其他症状:周身乏力及食欲减退,但无恶心、呕吐、腹痛、夜尿增多、尿痛、血尿等不适。近1个月来疼痛较前明显加重。
2﹒电解质 血钙明显升高(3.62mmol/L ↑),血磷低(0.53mmol/L ↓),Mg 0﹒48mmol/L ↓,24小时尿钙6.52mmol/L,磷7.8mmol/L。
3﹒血清PT H 191﹒0p mol/L ↑。
4﹒肝、肾功能正常。
5﹒蛋白芯片未见异常。
6﹒甲状旁腺核素扫描示甲状腺左叶上极区异常核素聚集,考虑为功能亢进的甲状旁腺组织。脑电图结果示脑电图广泛轻度异常,脑电地形图广泛轻度异常。
7﹒术后病理示甲状旁腺腺瘤,术后血钙恢复正常。
用药分析与药学监护
无症状的轻度高钙血症可以暂不采取控制血钙的措施;有症状体征的中度高钙血症要立即治疗;当患者血钙≥3.5mmol/L(14mg/dl)者,不论有无症状均需立即采取措施,降低血钙,维持机体内环境的稳定,减少并发症,为手术治疗争取机会。
1﹒扩容、促进尿钙排泄
(1)生理盐水:
高钙危象时易引起脱水,补充生理盐水可纠正脱水,并通过增加肾小球钙的滤过率及降低肾脏近、远曲小管对钠和钙的重吸收,使尿钙排泄增多。轻者可增加口服液体量和含氯化钠的饮食;重者通常采用0.9%氯化钠注射液静脉滴注,开始24~48小时每日持续静脉滴注3 000~4 000ml,可使血钙降低0.25~0.75mmol/L(200 ml/h),可同时增加口服补液量。大量补液须注意心、肺功能,以免诱发心力衰竭、肺水肿,老年患者及心、肾功能不全的患者使用时要特别慎重。另外,钙与洋地黄对心肌和传导系统有协同毒性作用,治疗中如须用洋地黄时,用量要酌减。
(2)利尿:
细胞外液容量补足后可使用呋塞米。呋塞米可作用于肾小管髓袢升支粗段,抑制钠和钙的重吸收,促进尿钙排泄。同时防止细胞外液容量补充过多,在积极输注生理盐水的同时应给予袢利尿剂,呋塞米应用剂量为20~40 mg静脉注射;当给予大剂量呋塞米加强治疗(80~120 mg/2~3h)时,需注意水和电解质补充,最好能监测中心静脉压、血及尿电解质,以防发生水、电解质紊乱和心力衰竭的发生,存在低钾血症时或低钾血症倾向时应注意补充钾盐。由于噻嗪类利尿药可减少肾脏钙的排泄,加重高血钙,故禁用噻嗪类利尿剂。
2﹒抑制骨吸收药物的应用
(1)双膦酸盐制剂:
静脉使用双膦酸盐是迄今为止最有效的治疗高钙血症的方法。高钙血症一经明确,必须尽早开始使用,因为双膦酸盐起效需2~4天,达到最大效果需4~7天,60%~70%患者血钙能降至正常水平,效果可持续1~4周。双膦酸盐胃肠道吸收率很低,因此治疗高钙血症时常采用静脉滴注给药。静脉注射时,将一定剂量双膦酸盐溶解于500ml以上的溶液中静脉滴注,维持4小时以上,以防双膦酸盐和钙的复合物沉积造成肾损害。目前用于治疗高钙血症的双膦酸盐有帕米膦酸钠、唑来膦酸、伊班膦酸盐、氯甲膦酸盐等。目前主要用帕米膦酸钠(pamidronate sodium),推荐剂量为30~60mg溶于500ml生理盐水中,静脉缓慢输入(时间6~8小时)。副作用为静脉滴注当日有肌肉酸痛,部分患者次日出现暂时性发热,偶有暂时性白细胞降低、轻度无症状低钙及低磷血症。效果呈剂量依赖性,重危患者可予90 mg。肾衰竭和高血磷时禁用。
(2)降钙素:
可抑制破骨细胞骨吸收,同时能减少肾小管钙的重吸收,增加尿钙排泄。起效快,但效果不如双膦酸盐显著。使用降钙素2~6小时内血钙可平均下降0.5mmol/L,但不能使大多数患者的血钙水平降至正常。常用剂量为鲑鱼降钙素2~8U/kg,鳗鱼降钙素0.4~1.6U/kg,均为皮下或肌内注射,每6~12小时重复注射,停药后24小时内血钙水平回升。重复注射时应酌情增加剂量,如应用同一剂量的降钙素不能达到首次注射的降血钙效果,有逸脱现象。降钙素的使用非常安全,少数患者仅有暂时性的轻度恶心、腹痛、肌痛及面色潮红。将降钙素与双膦酸盐联合使用,能够迅速和大幅度地降低血钙水平,且效果持久。
3﹒糖皮质激素
糖皮质激素通过多种途径达到降血钙水平的目的,如抑制肠钙吸收、增加尿钙排泄等,适用于血液系统恶性肿瘤如淋巴瘤和多发性骨髓瘤导致的高钙血症,也用于治疗维生素D或维生素A中毒或肉芽肿病导致的血钙水平升高。通常对实性肿瘤或原发性甲旁亢引发的高钙血症无效。常用剂量为氢化可的松200~300mg每日静脉滴注,一般3~5天。
4﹒其他
危急状态下,也可应用无钙透析液作腹膜透析、血液透析等以降低血钙水平。卧床的患者应尽早活动,以避免和缓解长期卧床造成的高钙血症。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#椎间盘突出#
25
#腰椎#
23
#腰椎间盘#
19
学习了.谢谢分享.
47
学习了.不错的病例
46
阅
43